4 Health Psychology: Sleep, Stress, and Sex
This chapter will discuss issues related to our health and well-being, with a particular emphasis on sleep, stress, and sexual behavior. The different stages of sleep will be identified, and sleep disorders will be described. Stress and coping strategies will then be discussed and reviewed. The chapter will close with discussions of sexual health and previous research on the sexual response cycle.
Table of Contents
4.1 Biological Rhythms and Sleep
4.4 Sleep Problems and Disorders
10.3 Sexual Health and Gender Identity
Biological Rhythms and Sleep
Biological Rhythms and Sleep Learning Objectives
By the end of this section, you will be able to:
- Explain how circadian rhythms are involved in regulating the sleep-wake cycle
- Describe how circadian cycles can be disrupted
- Discuss how circadian cycles can differ between individuals
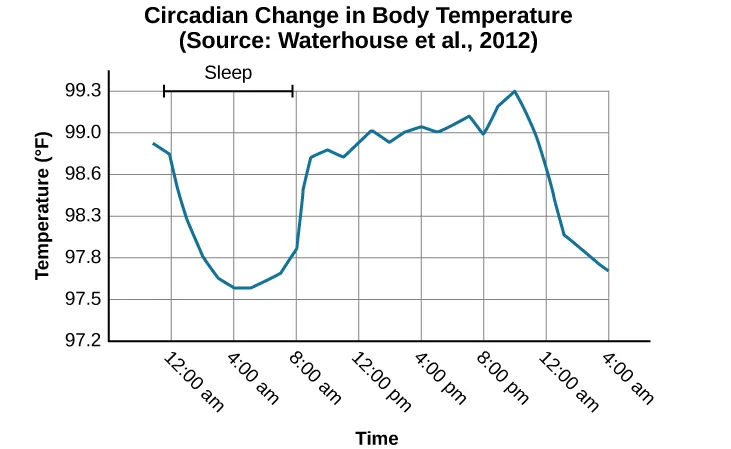
Biological rhythms are internal rhythms of biological activity. A woman’s menstrual cycle is an example of a biological rhythm—a recurring, cyclical pattern of bodily changes. One complete menstrual cycle takes about 28 days—a lunar month—but many biological cycles are much shorter. For example, body temperature fluctuates cyclically over a 24-hour period (Figure 4.2). Alertness is associated with higher body temperatures and sleepiness with lower body temperatures.
This temperature fluctuation pattern, which repeats daily, is one example of a circadian rhythm. A circadian rhythm is a biological rhythm that takes place over a period of about 24 hours. Our sleep-wake cycle, which is linked to our environment’s natural light-dark cycle, is perhaps the most obvious example of a circadian rhythm, but we also have daily fluctuations in heart rate, blood pressure, blood sugar, and body temperature.
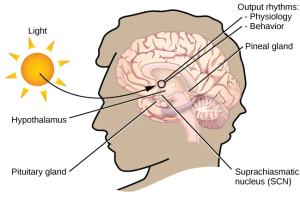
If we have biological rhythms, then is there some sort of biological clock? In the brain, the hypothalamus, which lies above the pituitary gland, is a main center of homeostasis. Homeostasis is the tendency to maintain a balance, or optimal level, within a biological system.
The brain’s clock mechanism is located in an area of the hypothalamus known as the suprachiasmatic nucleus (SCN). The axons of light-sensitive neurons in the retina provide information to the SCN based on the amount of light present, allowing this internal clock to be synchronized with the outside world (Klein, Moore, & Reppert, 1991; Welsh, Takahashi, & Kay, 2010) (Figure 4.3).
Problems With Circadian Rhythms
Generally, our circadian cycles are aligned with the outside world. For example, most people sleep during the night and are awake during the day. One important regulator of sleep-wake cycles is the hormone melatonin. The pineal gland, an endocrine structure located inside the brain that releases melatonin, is thought to be involved in regulating various biological rhythms and the immune system during sleep (Hardeland, Pandi-Perumal, & Cardinali, 2006). Melatonin release is stimulated by darkness and inhibited by light.
There are individual differences in regard to our sleep-wake cycle. For instance, some people would say they are morning people, while others consider themselves night owls. These individual differences in circadian patterns of activity are known as a person’s chronotype, and research demonstrates that morning larks and night owls differ with regard to sleep regulation (Taillard, Philip, Coste, Sagaspe, & Bioulac, 2003). Sleep regulation refers to the brain’s control of switching between sleep and wakefulness as well as coordinating this cycle with the outside world.
Disruptions of Normal Sleep
Whether lark, owl, or somewhere in between, there are situations in which a person’s circadian clock gets out of synchrony with the external environment. One way that this happens involves traveling across multiple time zones. When we do this, we often experience jet lag. Jet lag is a collection of symptoms that results from the mismatch between our internal circadian cycles and our environment. These symptoms include fatigue, sluggishness, irritability, and insomnia (i.e., a consistent difficulty in falling or staying asleep for at least three nights a week over a month’s time) (Roth, 2007).
Individuals who do rotating shift work are also likely to experience disruptions in circadian cycles. Rotating shift work refers to a work schedule that changes from early to late on a daily or weekly basis. For example, a person may work from 7:00 a.m. to 3:00 p.m. on Monday, 3:00 a.m. to 11:00 a.m. on Tuesday, and 11:00 a.m. to 7:00 p.m. on Wednesday. In such instances, the individual’s schedule changes so frequently that maintaining a normal circadian rhythm becomes difficult. This often results in sleeping problems, leading to signs of depression and anxiety. These kinds of schedules are common for individuals working in healthcare professions and service industries, and they are associated with persistent feelings of exhaustion and agitation that can make someone more prone to making mistakes on the job (Gold et al., 1992; Presser, 1995).
Rotating shift work has pervasive effects on the lives and experiences of individuals engaged in that kind of work, which is clearly illustrated in stories reported in a qualitative study that researched the experiences of middle-aged nurses who worked rotating shifts (West, Boughton & Byrnes, 2009). Several of the nurses interviewed commented that their work schedules affected their relationships with their families. One of the nurses said,
If you’ve had a partner who does work regular job 9 to 5 office hours . . . the ability to spend time, good time with them when you’re not feeling absolutely exhausted . . . that would be one of the problems that I’ve encountered. (West et al., 2009, p. 114)

While disruptions in circadian rhythms can have negative consequences, there are things we can do to help us realign our biological clocks with the external environment. Some of these approaches, such as using a bright light as shown in Figure 4.4, have been shown to alleviate some of the problems experienced by individuals suffering from jet lag or from the consequences of rotating shift work. Because the biological clock is driven by light, exposure to bright light during working shifts and dark exposure when not working can help combat insomnia and symptoms of anxiety and depression (Huang, Tsai, Chen, & Hsu, 2013).
Sleep and Why we sleep
Sleep and Why We Sleep Learning Objectives
By the end of this section, you will be able to:
- Describe areas of the brain involved in sleep
- Understand hormone secretions associated with sleep
- Describe several theories aimed at explaining the function of sleep
We spend approximately one-third of our lives sleeping. Given the average life expectancy for U.S. citizens falls between 73 and 79 years old (Singh & Siahpush, 2006), we can expect to spend approximately 25 years of our lives sleeping. Some animals never sleep (e.g., some fish and amphibian species); other animals sleep very little without apparent negative consequences (e.g., giraffes); yet some animals (e.g., rats) die after two weeks of sleep deprivation (Siegel, 2008). Why do we devote so much time to sleep? Is it absolutely essential that we sleep? This section will consider these questions and explore various explanations for why we sleep.
What is Sleep?
Sleep is distinguished by low levels of physical activity and reduced sensory awareness. As discussed by Siegel (2008), a definition of sleep must also include a mention of the interplay of the circadian and homeostatic mechanisms that regulate sleep. Homeostatic regulation of sleep is evidenced by sleep rebound following sleep deprivation. Sleep rebound refers to the fact that a sleep-deprived individual will fall asleep more quickly during subsequent opportunities for sleep. Sleep is characterized by certain brain activity patterns that can be visualized using electroencephalography (EEG), and different phases of sleep can be differentiated using EEG as well.
Sleep-wake cycles seem to be controlled by multiple brain areas acting in conjunction with one another. Some of these areas include the thalamus, the hypothalamus, and the pons. As already mentioned, the hypothalamus contains the SCN—the biological clock of the body—in addition to other nuclei that, in conjunction with the thalamus, regulate slow-wave sleep. The pons is important for regulating rapid eye movement (REM) sleep (National Institutes of Health, n.d.).
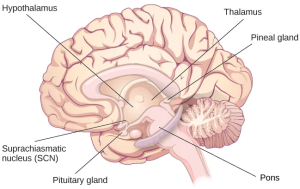
Sleep is also associated with the secretion and regulation of a number of hormones from several endocrine glands, including melatonin, follicle-stimulating hormone (FSH), luteinizing hormone (LH), and growth hormone (National Institutes of Health, n.d.). You have read that the pineal gland releases melatonin during sleep (Figure 4.6). Melatonin is thought to be involved in regulating various biological rhythms and the immune system (Hardeland et al., 2006). During sleep, the pituitary gland secretes FSH and LH, which are important in regulating the reproductive system (Christensen et al., 2012; Sofikitis et al., 2008). The pituitary gland also secretes growth hormone during sleep, which plays a role in physical growth, maturation, and other metabolic processes (Bartke, Sun, & Longo, 2013).
Why Do We Sleep?
Given the central role that sleep plays in our lives and the number of adverse consequences that have been associated with sleep deprivation, one would think that we would have a clear understanding of why it is that we sleep. Unfortunately, this is not the case; however, several hypotheses have been proposed to explain the function of sleep.
Adaptive Function of Sleep
One popular hypothesis of sleep incorporates the perspective of evolutionary psychology. Evolutionary psychology is a discipline that studies how universal patterns of behavior and cognitive processes have evolved over time as a result of natural selection. Variations and adaptations in cognition and behavior make individuals more or less successful in reproducing and passing their genes to their offspring. One hypothesis from this perspective might argue that sleep is essential to restore resources that are expended during the day. Just as bears hibernate in the winter when resources are scarce, perhaps people sleep at night to reduce their energy expenditures. While this is an intuitive explanation of sleep, little research supports this explanation. In fact, it has been suggested that there is no reason to think that energetic demands could not be addressed with periods of rest and inactivity (Frank, 2006; Rial et al., 2007), and some research has actually found a negative correlation between energetic demands and the amount of time spent sleeping (Capellini, Barton, McNamara, Preston, & Nunn, 2008).
Another evolutionary hypothesis of sleep holds that our sleep patterns evolved as an adaptive response to predatory risks, which increase in darkness. Thus we sleep in safe areas to reduce the chance of harm. Again, this is an intuitive and appealing explanation for why we sleep. Perhaps our ancestors spent extended periods of time asleep to reduce attention to themselves from potential predators. Comparative research indicates, however, that the relationship that exists between predatory risk and sleep is very complex and equivocal. Some research suggests that species that face higher predatory risks sleep fewer hours than other species (Capellini et al., 2008), while other researchers suggest there is no relationship between the amount of time a given species spends in deep sleep and its predation risk (Lesku, Roth, Amlaner, & Lima, 2006).
It is quite possible that sleep serves no single universally adaptive function, and different species have evolved different patterns of sleep in response to their unique evolutionary pressures. While we have discussed the negative outcomes associated with sleep deprivation, it should be pointed out that many benefits are associated with adequate amounts of sleep. A few such benefits listed by the National Sleep Foundation (n.d.) include maintaining a healthy weight, lowering stress levels, improving mood, and increasing motor coordination, as well as a number of benefits related to cognition and memory formation.
Cognitive Function of Sleep
Another theory regarding why we sleep involves sleep’s importance for cognitive function and memory formation (Rattenborg, Lesku, Martinez-Gonzalez, & Lima, 2007). Indeed, sleep deprivation results in disruptions in cognition and memory deficits (Brown, 2012), leading to impairments in our abilities to maintain attention, make decisions, and recall long-term memories. Moreover, these impairments become more severe as the amount of sleep deprivation increases (Alhola & Polo-Kantola, 2007). Furthermore, slow-wave sleep after learning a new task can improve resultant performance on that task (Huber, Ghilardi, Massimini, & Tononi, 2004) and seems essential for effective memory formation (Stickgold, 2005). Understanding the impact of sleep on cognitive function should help you understand that cramming all night for a test may be ineffective and can even prove counterproductive.
Getting the optimal amount of sleep has also been associated with other cognitive benefits. Research indicates that included among these possible benefits are increased capacities for creative thinking (Cai, Mednick, Harrison, Kanady, & Mednick, 2009; Wagner, Gais, Haider, Verleger, & Born, 2004), language learning (Fenn, Nusbaum, & Margoliash, 2003; Gómez, Bootzin, & Nadel, 2006), and inferential judgments (Ellenbogen, Hu, Payne, Titone, & Walker, 2007). It is possible that even the processing of emotional information is influenced by certain aspects of sleep (Walker, 2009).
Stages of Sleep
Stages of Sleep Learning Objectives
By the end of this section, you will be able to:
- Differentiate between REM and non-REM sleep
- Describe the differences between the three stages of non-REM sleep
- Understand the role that REM and non-REM sleep play in learning and memory
- Understand recommended amounts of sleep and the impact of sleep debt
Sleep is not a uniform state of being. Instead, sleep is composed of several different stages that can be differentiated from one another by the patterns of brain wave activity that occur during each stage. These changes in brain wave activity can be visualized using EEG and are distinguished from one another by both the frequency and amplitude of brain waves (Figure 4.7). Sleep can be divided into two different general phases: REM sleep and non-REM (NREM) sleep. Rapid eye movement (REM) sleep is characterized by darting movements of the eyes under closed eyelids. Brain waves during REM sleep appear very similar to brain waves during wakefulness. In contrast, non-REM (NREM) sleep is subdivided into four stages distinguished from each other and from wakefulness by characteristic patterns of brain waves. The first three stages of sleep are NREM sleep, while the fourth and final stage of sleep is REM sleep. In this section, we will discuss each of these stages of sleep and their associated patterns of brain wave activity.
NREM Stages of Sleep
The first stage of NREM sleep is known as stage 1 sleep. Stage 1 sleep is a transitional phase that occurs between wakefulness and sleep, the period during which we drift off to sleep. During this time, there is a slowdown in respiration and heartbeat rates. In addition, stage 1 sleep involves a marked decrease in overall muscle tension and core body temperature.
Regarding brain wave activity, stage 1 sleep is associated with alpha and theta waves. The early portion of stage 1 sleep produces alpha waves, which are relatively low frequency (8–13Hz), high amplitude patterns of electrical activity (waves) that become synchronized (Figure 4.8). This pattern of brain wave activity resembles that of someone who is very relaxed yet awake. As an individual continues through stage 1 sleep, there is an increase in theta wave activity. Theta waves are even lower frequency (4–7 Hz), higher amplitude brain waves than alpha waves. It is relatively easy to wake someone from stage 1 sleep; in fact, people often report that they have not been asleep if they are awoken during stage 1 sleep.
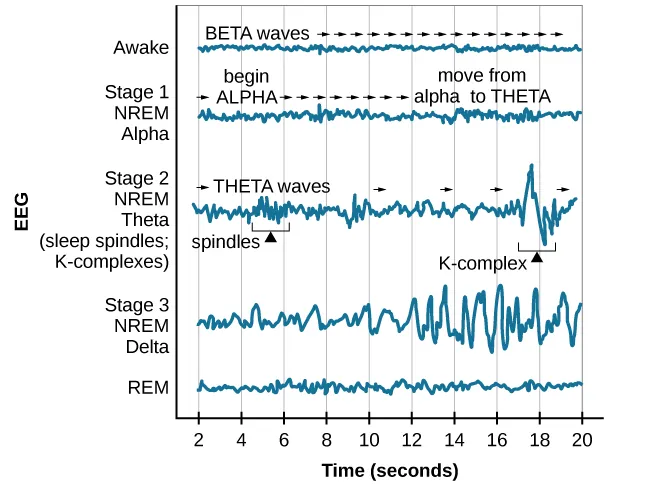
As we move into stage 2 sleep, the body goes into a state of deep relaxation. Theta waves still dominate the brain’s activity but are interrupted by brief bursts of activity known as sleep spindles (Figure 4.8). A sleep spindle is a rapid burst of higher-frequency brain waves that may be important for learning and memory (Fogel & Smith, 2011; Poe, Walsh, & Bjorness, 2010). In addition, the appearance of K-complexes is often associated with stage 2 sleep. A K-complex is a very high amplitude pattern of brain activity that may, in some cases, occur in response to environmental stimuli. Thus, K-complexes might serve as a bridge to higher levels of arousal in response to what is going on in our environments (Halász, 1993; Steriade & Amzica, 1998).
Stage 3 is often referred to as deep sleep or slow-wave sleep because this stage is characterized by low frequency (less than 3 Hz) and high amplitude delta waves (Figure 4.8). During this time, an individual’s heart rate and respiration slow dramatically. It is much more difficult to awaken someone from sleep during stage 3 than during earlier stages. Interestingly, individuals who have increased levels of alpha brain wave activity (more often associated with wakefulness and transition into stage 1 sleep) during stage 3 often report that they do not feel refreshed upon waking, regardless of how long they slept (Stone, Taylor, McCrae, Kalsekar, & Lichstein, 2008).
REM Sleep
As mentioned earlier, REM sleep is marked by rapid movements of the eyes. The brain waves associated with this stage of sleep are very similar to those observed when a person is awake, as shown in Figure 4.8, and this is the period of sleep in which dreaming occurs. It is also associated with paralysis of muscle systems in the body, with the exception of those that make circulation and respiration possible. Therefore, no movement of voluntary muscles occurs during REM sleep in a normal individual; REM sleep is often called paradoxical sleep because of this combination of high brain activity and lack of muscle tone. Like NREM sleep, REM has been implicated in various aspects of learning and memory (Wagner, Gais, & Born, 2001; Siegel, 2001).
If people are deprived of REM sleep and then allowed to sleep without disturbance, they will spend more time in REM sleep in what would appear to be an effort to recoup the lost time in REM. This is known as the REM rebound, and it suggests that REM sleep is also homeostatically regulated. Aside from the role that REM sleep may play in processes related to learning and memory, REM sleep may also be involved in emotional processing and regulation. In such instances, REM rebound may actually represent an adaptive response to stress in non-depressed individuals by suppressing the emotional salience of aversive events that occurred in wakefulness (Suchecki, Tiba, & Machado, 2012). Sleep deprivation, in general, is associated with a number of negative consequences (Brown, 2012).
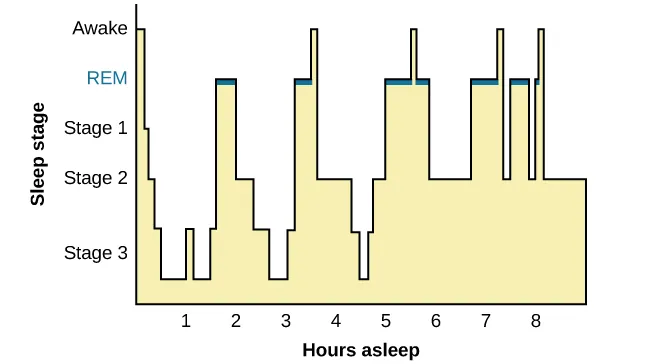
The hypnogram below (Figure 4.12) shows a person’s passage through the stages of sleep.
Dreams
Dreams and their associated meanings vary across different cultures and periods of time. By the late 19th century, German psychiatrist Sigmund Freud had become convinced that dreams represented an opportunity to gain access to the unconscious. By analyzing dreams, Freud thought people could increase self-awareness and gain valuable insight to help them deal with the problems they faced in their lives. Freud made distinctions between the manifest content and the latent content of dreams. Manifest content is the actual content, or storyline, of a dream. Latent content, on the other hand, refers to the hidden meaning of a dream. For instance, if an individual dreams about being chased by a snake, Freud might have argued that this represents the person’s fear of sexual intimacy, with the snake serving as a symbol of a penis.
The sleep and dreaming researcher Rosalind Cartwright, however, believes that dreams simply reflect life events that are important to the dreamer. Unlike Freud, Cartwright’s ideas about dreaming have found empirical support. For example, she and her colleagues published a study in which women going through divorce were asked several times over a five-month period to report the degree to which their former spouses were on their minds. These women were awakened during REM sleep to provide a detailed account of their dream content. There was a significant positive correlation between the degree to which women thought about their former spouses during waking hours and the number of times their former spouses appeared as characters in their dreams (Cartwright, Agargun, Kirkby, & Friedman, 2006). Recent research (Horikawa, Tamaki, Miyawaki, & Kamitani, 2013) has uncovered new techniques by which researchers may effectively detect and classify the visual images that occur during dreaming by using fMRI for neural measurement of brain activity patterns, opening the way for additional research in this area.
Insufficient Sleep
When people have difficulty getting sleep due to their work or the demands of day-to-day life, they accumulate sleep debt. A person with a sleep debt does not get sufficient sleep on a chronic basis. The consequences of sleep debt include decreased levels of alertness and mental efficiency. Interestingly, since the advent of electric light, the amount of sleep that people get has declined. While we certainly welcome the convenience of having the darkness lit up, we also suffer the consequences of reduced amounts of sleep because we are more active during the nighttime hours than our ancestors were. As a result, many of us sleep less than 7–8 hours a night and accrue a sleep debt. While there is tremendous variation in any given individual’s sleep needs, the National Sleep Foundation (n.d.) cites research to estimate that newborns require the most sleep (between 12 and 18 hours a night) and that this amount declines to just 7–9 hours by the time we are adults.
If you lie down to nap and fall asleep very easily, you may have a sleep debt. Given that college students are notorious for suffering from significant sleep debt (Hicks, Fernandez, & Pelligrini, 2001; Hicks, Johnson, & Pelligrini, 1992; Miller, Shattuck, & Matsangas, 2010), chances are you and your classmates deal with sleep debt-related issues on a regular basis. In 2015, the National Sleep Foundation updated their sleep duration hours to accommodate individual differences better. Table 4.1 shows the new recommendations, which describe sleep durations that are “recommended,” “may be appropriate,” and “not recommended.”
| Sleep Needs at Different Ages | |||
|---|---|---|---|
| Age | Recommended | May be appropriate | Not recommended |
| 0–3 months | 14–17 hours | 11–13 hours 18–19 hours |
Fewer than 11 hours More than 19 hours |
| 4–11 months | 12–15 hours | 10–11 hours 16–18 hours |
Fewer than 10 hours More than 18 hours |
| 1–2 years | 11–14 hours | 9–10 hours 15–16 hours |
Fewer than 9 hours More than 16 hours |
| 3–5 years | 10–13 hours | 8–9 hours 14 hours |
Fewer than 8 hours More than 14 hours |
| 6–13 years | 9–11 hours | 7–8 hours 12 hours |
Fewer than 7 hours More than 12 hours |
| 14–17 years | 8–10 hours | 7 hours 11 hours |
Fewer than 7 hours More than 11 hours |
| 18–25 years | 7–9 hours | 6 hours 10–11 hours |
Fewer than 6 hours More than 11 hours |
| 26–64 years | 7–9 hours | 6 hours 10 hours |
Fewer than 6 hours More than 10 hours |
| ≥65 years | 7–8 hours | 5–6 hours 9 hours |
Fewer than 5 hours More than 9 hours |
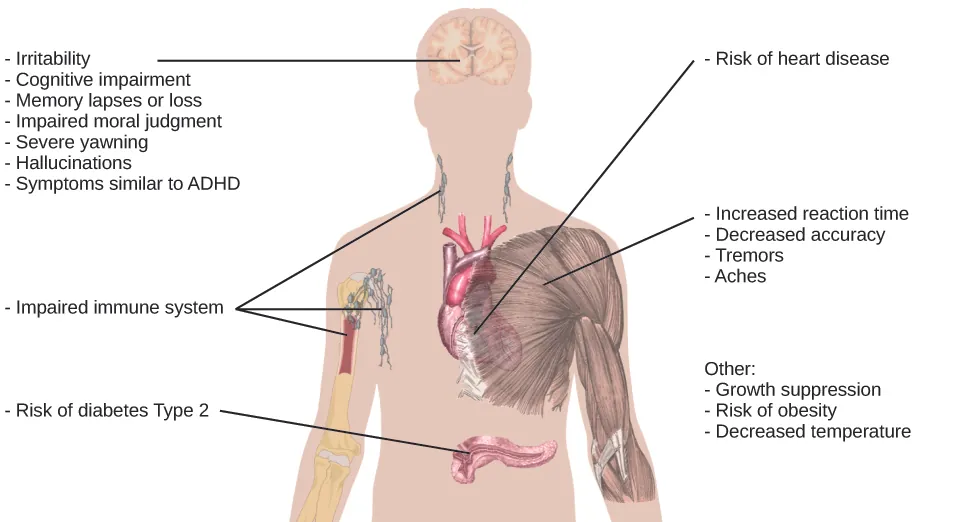
Sleep debt and sleep deprivation have significant negative psychological and physiological consequences Figure 4.5. As mentioned, lack of sleep can decrease mental alertness and cognitive function. In addition, sleep deprivation often results in depression-like symptoms. These effects can occur as a function of accumulated sleep debt or in response to more acute periods of sleep deprivation. It may surprise you that sleep deprivation is associated with obesity, increased blood pressure, increased levels of stress hormones, and reduced immune functioning (Banks & Dinges, 2007).
A sleep-deprived individual generally will fall asleep more quickly than if they were not sleep deprived. Some sleep-deprived individuals have difficulty staying awake when they stop moving (for example, sitting and watching television or driving a car). That is why individuals suffering from sleep deprivation can also put themselves and others at risk when they put themselves behind the wheel of a car or work with dangerous machinery. Some research suggests that sleep deprivation affects cognitive and motor function as much as, if not more than, alcohol intoxication (Williamson & Feyer, 2000).
Research shows that the most severe effects of sleep deprivation occur when a person stays awake for more than 24 hours (Killgore & Weber, 2014; Killgore et al., 2007) or following repeated nights with fewer than four hours in bed (Wickens, Hutchins, Lauk, Seebook, 2015). For example, irritability, distractibility, and impairments in cognitive and moral judgment can occur with fewer than four hours of sleep. If someone stays awake for 48 consecutive hours, they could start to hallucinate.
The amount of sleep we get varies across the lifespan. We spend up to 16 hours a day sleeping when we are very young. As we grow older, we sleep less. In fact, a meta-analysis, which is a study that combines the results of many related studies, conducted within the last decade indicates that by the time we are 65 years old, we average fewer than 7 hours of sleep per day (Ohayon, Carskadon, Guilleminault, & Vitiello, 2004).
Sleep Problems and Disorders
Sleep Problems and Disorders Learning Objectives
By the end of this section, you will be able to:
- Describe the symptoms and treatments of insomnia
- Recognize the symptoms of several parasomnias
- Describe the symptoms and treatments for narcolepsy
Many people experience disturbances in their sleep at some point in their lives. Depending on the population and sleep disorder being studied, between 30% and 50% of the population suffers from a sleep disorder at some point in their lives (Bixler, Kales, Soldatos, Kaels, & Healey, 1979; Hossain & Shapiro, 2002; Ohayon, 1997, 2002; Ohayon & Roth, 2002). This section will describe several sleep disorders and some of their treatment options.
Insomnia
Insomnia, a consistent difficulty in falling or staying asleep, is the most common of the sleep disorders. Individuals with insomnia often experience long delays between the times that they go to bed and actually fall asleep. In addition, these individuals may wake up several times during the night only to find that they have difficulty getting back to sleep. As mentioned earlier, one of the criteria for insomnia involves experiencing these symptoms for at least three nights a week for at least one month’s time (Roth, 2007).
It is not uncommon for people suffering from insomnia to experience increased levels of anxiety about their inability to fall asleep. This becomes a self-perpetuating cycle because increased anxiety leads to increased arousal, and higher levels of arousal make the prospect of falling asleep even more unlikely. Chronic insomnia is almost always associated with feeling overtired and may be associated with symptoms of depression.
Many factors may contribute to insomnia, including age, drug use, exercise, mental status, and bedtime routines. Not surprisingly, insomnia treatment may take one of several different approaches. People who suffer from insomnia might limit their use of stimulant drugs (such as caffeine) or increase their amount of physical exercise during the day. Some people might turn to over-the-counter (OTC) or prescribed sleep medications to help them sleep, but this should be done sparingly because many sleep medications result in dependence and alter the nature of the sleep cycle, and they can increase insomnia over time. Those who continue to have insomnia, particularly if it affects their quality of life, should seek professional treatment.
Some forms of psychotherapy, such as cognitive-behavioral therapy, can help sufferers of insomnia. Cognitive-behavioral therapy (CBT) is a type of psychotherapy focusing on cognitive processes and problem behaviors. The treatment of insomnia likely would include stress management techniques and changes in problematic behaviors that could contribute to insomnia (e.g., spending more waking time in bed). Cognitive-behavioral therapy has been demonstrated to be quite effective in treating insomnia (Savard, Simard, Ivers, & Morin, 2005; Williams, Roth, Vatthauer, & McCrae, 2013).
EVERYDAY CONNECTION: Solutions to Support Healthy Sleep
Has something like this ever happened to you? My sophomore college housemate got so stressed out during finals sophomore year that he drank almost a whole bottle of Nyquil to try to fall asleep. When he told me, I made him go see the college therapist.
Many college students struggle to get the recommended 7–9 hours of sleep each night. However, for some, it’s not because of all-night partying or late-night study sessions. It’s simply that they feel so overwhelmed and stressed that they cannot fall asleep or stay asleep. One or two nights of sleep difficulty is not unusual, but if you experience anything more than that, you should seek a doctor’s advice.
Here are some tips for maintaining healthy sleep:
- Stick to a sleep schedule, even on the weekends. Try going to bed and waking up at the same time every day to keep your biological clock in sync so your body gets in the habit of sleeping every night.
- Avoid anything stimulating for an hour before bed. That includes exercise and bright light from devices.
- Exercise daily.
- Avoid naps.
- Keep your bedroom temperature between 60 and 67 degrees. People sleep better in cooler temperatures.
- Avoid alcohol, cigarettes, caffeine, and heavy meals before bed. It may feel like alcohol helps you sleep, but it actually disrupts REM sleep and leads to frequent awakenings. Heavy meals may make you sleepy, but they can also lead to frequent awakenings due to gastric distress.
- If you cannot fall asleep, leave your bed and do something else until you feel tired again. Train your body to associate the bed with sleeping rather than other activities like studying, eating, or watching television shows.
Parasomnias
Parasomnias are one of a group of sleep disorders in which unwanted, disruptive motor activity and/or experiences during sleep play a role. Parasomnias can occur in either REM or NREM phases of sleep. Sleepwalking, restless leg syndrome, and night terrors are all examples of parasomnias (Mahowald & Schenck, 2000).
Sleepwalking
In sleepwalking or somnambulism, the sleeper engages in relatively complex behaviors ranging from wandering about to driving a car. During periods of sleepwalking, sleepers often have their eyes open, but they are not responsive to attempts to communicate with them. Sleepwalking most often occurs during slow-wave sleep, but it can occur at any time during a sleep period in some affected individuals (Mahowald & Schenck, 2000).
Historically, somnambulism has been treated with a variety of pharmacotherapies ranging from benzodiazepines to antidepressants. However, the success rate of such treatments is questionable. Guilleminault et al. (2005) found that sleepwalking was not alleviated with the use of benzodiazepines. However, all of their somnambulistic patients who also suffered from sleep-related breathing problems showed a marked decrease in sleepwalking when their breathing problems were effectively treated.
DIG DEEPER: A Sleepwalking Defense?
On January 16, 1997, Scott Falater sat down to dinner with his wife and children and told them about difficulties he was experiencing on a project at work. After dinner, he prepared some materials to use in leading a church youth group the following morning, and then he attempted to repair the family’s swimming pool pump before retiring to bed. The following morning, he awoke to barking dogs and unfamiliar voices from downstairs. As he went to investigate what was going on, he was met by a group of police officers who arrested him for the murder of his wife (Cartwright, 2004; CNN, 1999).
Yarmila Falater’s body was found in the family’s pool with 44 stab wounds. A neighbor called the police after witnessing Falater standing over his wife’s body before dragging her into the pool. Upon a search of the premises, police found blood-stained clothes and a bloody knife in the trunk of Falater’s car, and he had blood stains on his neck.
Remarkably, Falater insisted that he had no recollection of hurting his wife in any way. His children and his wife’s parents all agreed that Falater had an excellent relationship with his wife and they couldn’t think of a reason that would provide any sort of motive to murder her (Cartwright, 2004).
Scott Falater had a history of regular episodes of sleepwalking as a child, and he had even behaved violently toward his sister once when she tried to prevent him from leaving their home in his pajamas during a sleepwalking episode. He suffered from no apparent anatomical brain anomalies or psychological disorders. It appeared that Scott Falater had killed his wife in his sleep, or at least, that is the defense he used when he was tried for his wife’s murder (Cartwright, 2004; CNN, 1999). In Falater’s case, a jury found him guilty of first degree murder in June of 1999 (CNN, 1999); however, there are other murder cases where the sleepwalking defense has been used successfully. As scary as it sounds, many sleep researchers believe that homicidal sleepwalking is possible in individuals suffering from the types of sleep disorders described below (Broughton et al., 1994; Cartwright, 2004; Mahowald, Schenck, & Cramer Bornemann, 2005; Pressman, 2007).
Other Parasomnias
A person with restless leg syndrome has uncomfortable sensations in the legs during periods of inactivity or when trying to fall asleep. This discomfort is relieved by deliberately moving the legs, which, not surprisingly, contributes to difficulty in falling or staying asleep. Restless leg syndrome is quite common and has been associated with a number of other medical diagnoses, such as chronic kidney disease and diabetes (Mahowald & Schenck, 2000). There are a variety of drugs that treat restless leg syndrome: benzodiazepines, opiates, and anticonvulsants (Restless Legs Syndrome Foundation, n.d.).
Night terrors result in a sense of panic in the sufferer and are often accompanied by screams and attempts to escape from the immediate environment (Mahowald & Schenck, 2000). Although individuals suffering from night terrors appear to be awake, they generally have no memories of the events that occurred, and attempts to console them are ineffective. Typically, individuals suffering from night terrors will fall back asleep again within a short time. Night terrors apparently occur during the NREM phase of sleep (Provini, Tinuper, Bisulli, & Lagaresi, 2011). Generally, treatment for night terrors is unnecessary unless there is some underlying medical or psychological condition that is contributing to the night terrors (Mayo Clinic, n.d.).
Narcolepsy
Unlike the other sleep disorders described in this section, a person with narcolepsy cannot resist falling asleep at inopportune times. These sleep episodes are often associated with cataplexy, which is a lack of muscle tone or muscle weakness, and in some cases, involves complete paralysis of the voluntary muscles. This is similar to the kind of paralysis experienced by healthy individuals during REM sleep (Burgess & Scammell, 2012; Hishikawa & Shimizu, 1995; Luppi et al., 2011). Narcoleptic episodes take on other features of REM sleep. For example, around one-third of individuals diagnosed with narcolepsy experience vivid, dream-like hallucinations during narcoleptic attacks (Chokroverty, 2010).
Surprisingly, narcoleptic episodes are often triggered by states of heightened arousal or stress. The typical episode can last from a minute or two to half an hour. Once awakened from a narcoleptic attack, people report feeling refreshed (Chokroverty, 2010). Obviously, regular narcoleptic episodes could interfere with the ability to perform one’s job or complete schoolwork, and in some situations, narcolepsy can result in significant harm and injury (e.g., driving a car or operating machinery or other potentially dangerous equipment).
Generally, narcolepsy is treated using psychomotor stimulant drugs, such as amphetamines (Mignot, 2012). These drugs promote increased levels of neural activity. Narcolepsy is associated with reduced levels of the signaling molecule hypocretin in some areas of the brain (De la Herrán-Arita & Drucker-Colín, 2012; Han, 2012), and the traditional stimulant drugs do not have direct effects on this system. Therefore, it is quite likely that new medications that are developed to treat narcolepsy will be designed to target the hypocretin system.
Sleep Review
What is stress?
Sleep can be hard to come by when we need it most. For example, when we are dealing with periods of chronic stress, we may struggle to fall asleep and stay asleep. What is stress? Why do we experience it? What are the consequences of acute and chronic stressors?
What is Stress? Learning Objectives
By the end of this section, you will be able to:
- Understand the physiological basis of stress and describe the general adaptation syndrome
- Describe different types of possible stressors
- Explain the importance of life changes as potential stressors
The Physiological Basis of Stress
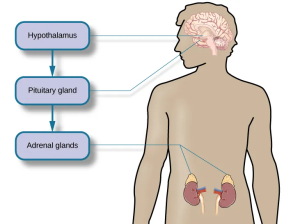
What goes on inside our bodies when we experience stress? The physiological mechanisms of stress are extremely complex, but they generally involve the work of two systems—the sympathetic nervous system and the hypothalamic-pituitary-adrenal (HPA) axis. When a person first perceives something as stressful (Selye’s alarm reaction), the sympathetic nervous system triggers arousal via the release of adrenaline from the adrenal glands. Release of these hormones activates the fight-or-flight responses to stress, such as accelerated heart rate and respiration. At the same time, the HPA axis, which is primarily endocrine in nature, becomes especially active, although it works much more slowly than the sympathetic nervous system. In response to stress, the hypothalamus (one of the limbic structures in the brain) releases corticotrophin-releasing factor, a hormone that causes the pituitary gland to release adrenocorticotropic hormone (ACTH) (Figure 4.13). The ACTH then activates the adrenal glands to secrete a number of hormones into the bloodstream; an important one is cortisol, which can affect virtually every organ within the body. Cortisol is commonly known as a stress hormone and helps provide that boost of energy when we first encounter a stressor, preparing us to run away or fight. However, sustained elevated levels of cortisol weaken the immune system.
In short bursts, this process can have some favorable effects, such as providing extra energy, improving immune system functioning temporarily, and decreasing pain sensitivity. However, extended release of cortisol—as would happen with prolonged or chronic stress—often comes at a high price. High levels of cortisol have been shown to produce a number of harmful effects. For example, increases in cortisol can significantly weaken our immune system (Glaser & Kiecolt-Glaser, 2005), and high levels are frequently observed among depressed individuals (Geoffroy, Hertzman, Li, & Power, 2013). In summary, a stressful event causes various physiological reactions that activate the adrenal glands, releasing epinephrine, norepinephrine, and cortisol. These hormones affect a number of bodily processes in ways that prepare the stressed person to take direct action but also in ways that may heighten the potential for illness.
When stress is extreme or chronic, it can have profoundly negative consequences. For example, stress often contributes to the development of certain psychological disorders, including post-traumatic stress disorder, major depressive disorder, and other serious psychiatric conditions. Additionally, we noted earlier that stress is linked to the development and progression of various physical illnesses and diseases. For example, researchers in one study found that people injured during the September 11, 2001, World Trade Center disaster or who developed post-traumatic stress symptoms afterward later suffered significantly elevated rates of heart disease (Jordan, Miller-Archie, Cone, Morabia, & Stellman, 2011). Another investigation yielded that self-reported stress symptoms among aging and retired Finnish food industry workers were associated with morbidity 11 years later. This study also predicted the onset of musculoskeletal, nervous system, and endocrine and metabolic disorders (Salonen, Arola, Nygård, & Huhtala, 2008). Another study reported that male South Korean manufacturing employees who reported high levels of work-related stress were more likely to catch the common cold over the next several months than were those employees who reported lower work-related stress levels (Park et al., 2011). Later, you will explore the mechanisms through which stress can produce physical illness and disease.
For an individual to experience stress, they must first encounter a potential stressor. Stressors can be placed into one of two broad categories: chronic and acute. Chronic stressors include events that persist over an extended period fo time, such as caring for a parent with dementia, long-term unemployment, or imprisonment. Acute stressors involve brief focal events that sometimes continue to be experienced as overwhelming well after the event has ended, such as falling on an icy sidewalk and breaking your leg (Cohen, Janice-Deverts, & Miller, 2007). Whether chronic or acute, potential stressors come in many shapes and sizes. They can include major traumatic events, significant life changes, daily hassles, as well as other situations in which a person is regularly exposed to threats, challenges, or danger.
Traumatic Events
Some stressors involve traumatic events or situations in which a person is exposed to actual or threatened death or serious injury. Stressors in this category include exposure to military combat, threatened or actual physical assaults (e.g., physical attacks, sexual assault, robbery, childhood abuse), terrorist attacks, natural disasters (e.g., earthquakes, floods, hurricanes), and automobile accidents. Men, non-Whites, and individuals in lower socioeconomic status (SES) groups report experiencing a greater number of traumatic events than do women, Whites, and individuals in higher SES groups (Hatch & Dohrenwend, 2007). Some individuals who are exposed to stressors of extreme magnitude develop post-traumatic stress disorder (PTSD): a chronic stress reaction characterized by experiences and behaviors that may include intrusive and painful memories of the stressor event, jumpiness, persistent negative emotional states, detachment from others, angry outbursts, and avoidance of reminders of the event (American Psychiatric Association [APA], 2013).
Life Changes
Most stressors we encounter are not nearly as intense as the ones described above. Many potential stressors we face involve events or situations that require us to make changes in our ongoing lives and require time as we adjust to those changes. Examples include the death of a close family member, marriage, divorce, and moving.
In the 1960s, psychiatrists Thomas Holmes and Richard Rahe wanted to examine the link between life stressors and physical illness, based on the hypothesis that life events requiring significant changes in a person’s normal life routines are stressful, whether these events are desirable or undesirable. They developed the Social Readjustment Rating Scale (SRRS), consisting of 43 life events that require varying degrees of personal readjustment (Holmes & Rahe, 1967). Many life events that most people would consider pleasant (e.g., holidays, retirement, marriage) are among those listed on the SRRS; these are examples of eustress. Holmes and Rahe also proposed that life events can add up over time, and that experiencing a cluster of stressful events increases one’s risk of developing physical illnesses.
In developing their scale, Holmes and Rahe asked 394 participants to provide a numerical estimate for each of the 43 items; each estimate corresponded to how much readjustment participants felt each event would require. These estimates resulted in mean value scores for each event—often called life change units (LCUs) (Rahe, McKeen, & Arthur, 1967). The numerical scores ranged from 11 to 100, representing the perceived magnitude of life change each event entails. Death of a spouse ranked highest on the scale with 100 LCUs, and divorce ranked second highest with 73 LCUs. In addition, personal injury or illness, marriage, and job termination also ranked highly on the scale with 53, 50, and 47 LCUs, respectively. Conversely, change in residence (20 LCUs), change in eating habits (15 LCUs), and vacation (13 LCUs) ranked low on the scale (Table 14.1). Minor violations of the law ranked the lowest with 11 LCUs. To complete the scale, participants checked yes for events experienced within the last 12 months. LCUs for each checked item are totaled for a score quantifying the amount of life change. Agreement on the amount of adjustment required by the various life events on the SRRS is highly consistent, even cross-culturally (Holmes & Masuda, 1974).
| Some Stressors on the Social Readjustment Rating Scale (Holmes & Rahe, 1967) | |
|---|---|
| Life event | Life change units |
| Death of a close family member | 63 |
| Personal injury or illness | 53 |
| Dismissal from work | 47 |
| Change in financial state | 38 |
| Change to different line of work | 36 |
| Outstanding personal achievement | 28 |
| Beginning or ending school | 26 |
| Change in living conditions | 25 |
| Change in working hours or conditions | 20 |
| Change in residence | 20 |
| Change in schools | 20 |
| Change in social activities | 18 |
| Change in sleeping habits | 16 |
| Change in eating habits | 15 |
| Minor violation of the law | 11 |
Extensive research has demonstrated that accumulating a high number of life change units within a brief period of time (one or two years) is related to a wide range of physical illnesses (even accidents and athletic injuries) and mental health problems (Monat & Lazarus, 1991; Scully, Tosi, & Banning, 2000).
Stress and Illness
Stress and Illness Learning Objectives
By the end of this section, you will be able to:
- Explain the nature of psychophysiological disorders
- Describe the immune system and how stress impacts its functioning
- Describe how stress and emotional factors can lead to the development and exacerbation of cardiovascular disorders, asthma, and tension headaches
In this section, we will discuss stress and illness. As stress researcher Robert Sapolsky (1998) describes, stress-related disease emerges predominantly out of the fact that we so often activate a physiological system that has evolved for responding to acute physical emergencies, but we turn it on for months on end, worrying about mortgages, relationships, and promotions. (p. 6)
The stress response, as noted earlier, consists of a coordinated but complex system of physiological reactions that are called upon as needed. These reactions are sometimes beneficial because they prepare us to deal with potentially dangerous or threatening situations (for example, recall our old friend, the fearsome bear on the trail). However, health is affected when physiological reactions are sustained, as can happen in response to ongoing stress.
Psychophysiological Disorders
If the reactions that compose the stress response are chronic or frequently exceed normal ranges, they can lead to cumulative wear and tear on the body, in much the same way that running your air conditioner on full blast all summer will eventually cause wear and tear on it. For example, the high blood pressure that a person under considerable job strain experiences might eventually take a toll on his heart and set the stage for a heart attack or heart failure. Also, someone exposed to high levels of the stress hormone cortisol might become vulnerable to infection or disease because of weakened immune system functioning (McEwen, 1998).
Physical disorders or diseases whose symptoms are brought about or worsened by stress and emotional factors are called psychophysiological disorders. The physical symptoms of psychophysiological disorders are real and can be produced or exacerbated by psychological factors (hence the psycho and physiological in psychophysiological). A list of frequently encountered psychophysiological disorders is provided in Table 14.3.
| Types of Psychophysiological Disorders (adapted from Everly & Lating, 2002) | |
|---|---|
| Type of Psychophysiological Disorder | Examples |
| Cardiovascular | hypertension, coronary heart disease |
| Gastrointestinal | irritable bowel syndrome |
| Respiratory | asthma, allergy |
| Musculoskeletal | low back pain, tension headaches |
| Skin | acne, eczema, psoriasis |
Below, we discuss two kinds of psychophysiological disorders about which a great deal is known: cardiovascular disorders and asthma. First, however, it is necessary to focus on a discussion of the immune system—one of the major pathways through which stress and emotional factors can lead to illness and disease.
EVERYDAY CONNECTION: Social Status, Stress, and Health Care
Psychologists have long been aware that social status (e.g., wealth, privilege) is intimately tied to stress, health, and well-being. Some factors that contribute to high stress and poor health among people with lower social status include lack of control and predictability (e.g., greater unemployment) and resource inequality (e.g., less access to health care and other community resources) (Marmot & Sapolsky, 2014).
In the United States, resource inequalities tied to social status often create race and gender differences in health care. For example, African American women have the highest rates of emergency room visits and unmet healthcare needs compared to any other group, and this disparity increased significantly from 2006 to 2014 (Manuel, 2018). Lesbian, gay, bisexual, and transgender youth often experience poor quality of care due to stigma, lack of understanding, and insensitivity among healthcare professionals (Hafeez, Zeshan, Tahir, Jahan, & Naveed, 2017). One goal of the U.S. government’s Healthy People 2020 initiative is to eliminate gender and race disparities in health care. Their interactive dataset provides an updated snapshot of health disparities: https://www.healthypeople.gov/2020/data-search/health-disparities-data.
Stress and the Immune System
In a sense, the immune system is the body’s surveillance system. It consists of a variety of structures, cells, and mechanisms that serve to protect the body from invading microorganisms that can harm or damage the body’s tissues and organs. When the immune system is working as it should, it keeps us healthy and disease free by eliminating harmful bacteria, viruses, and other foreign substances that have entered the body (Everly & Lating, 2002).
The question of whether stress and negative emotional states can influence immune function has captivated researchers for over three decades, and discoveries made over that time have dramatically changed the face of health psychology (Kiecolt-Glaser, 2009). Psychoneuroimmunology is the field that studies how psychological factors such as stress influence the immune system and immune functioning. The term psychoneuroimmunology was first coined in 1981, when it appeared as the title of a book that reviewed available evidence for associations between the brain, endocrine system, and immune system (Zacharie, 2009). To a large extent, this field evolved from discovering a connection between the central nervous system and the immune system.
Some of the most compelling evidence for a connection between the brain and the immune system comes from studies in which researchers demonstrated that immune responses in animals could be classically conditioned (Everly & Lating, 2002). For example, Ader and Cohen (1975) paired flavored water (the conditioned stimulus) with the presentation of an immunosuppressive drug (the unconditioned stimulus), causing sickness (an unconditioned response). Not surprisingly, rats exposed to this pairing developed a conditioned aversion to the flavored water. However, the taste of the water itself later produced immunosuppression (a conditioned response), indicating that the immune system itself had been conditioned. Many subsequent studies over the years have further demonstrated that immune responses can be classically conditioned in both animals and humans (Ader & Cohen, 2001). Thus, if classical conditioning can alter immunity, other psychological factors should be capable of altering it as well.
Hundreds of studies involving tens of thousands of participants have tested many kinds of brief and chronic stressors and their effects on the immune system (e.g., public speaking, medical school examinations, unemployment, marital discord, divorce, death of spouse, burnout and job strain, and caring for a relative with Alzheimer’s disease). It has been repeatedly demonstrated that many kinds of stressors are associated with poor or weakened immune functioning (Glaser & Kiecolt-Glaser, 2005; Kiecolt-Glaser, McGuire, Robles, & Glaser, 2002; Segerstrom & Miller, 2004).
When evaluating these findings, it is important to remember that there is a tangible physiological connection between the brain and the immune system. For example, the sympathetic nervous system innervates immune organs such as the thymus, bone marrow, spleen, and lymph nodes (Maier, Watkins, & Fleshner, 1994). Also, we noted earlier that stress hormones released during hypothalamic-pituitary-adrenal (HPA) axis activation can adversely impact immune function. One way they do this is by inhibiting the production of lymphocytes, white blood cells that circulate in the body’s fluids that are important in the immune response (Everly & Lating, 2002).
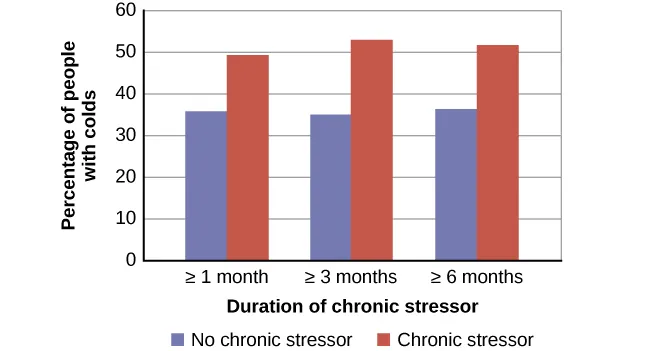
Some of the more dramatic examples demonstrating the link between stress and impaired immune function involve studies in which volunteers were exposed to viruses. The rationale behind this research is that because stress weakens the immune system, people with high stress levels should be more likely to develop an illness compared to those under little stress. In one memorable experiment using this method, researchers interviewed 276 healthy volunteers about recent stressful experiences (Cohen et al., 1998). Following the interview, these participants were given nasal drops containing the cold virus (in case you are wondering why anybody would ever want to participate in a study in which they are subjected to such treatment, the participants were paid $800 for their trouble). When examined later, participants who reported experiencing chronic stressors for more than one month—especially enduring difficulties involving work or relationships—were considerably more likely to have developed colds than participants who reported no chronic stressors (Figure 4.14).
In another study, older volunteers were given an influenza virus vaccination. Compared to controls, those who were caring for a spouse with Alzheimer’s disease (and thus were under chronic stress) showed poorer antibody response following the vaccination (Kiecolt-Glaser, Glaser, Gravenstein, Malarkey, & Sheridan, 1996).
Other studies have demonstrated that stress slows wound healing by impairing immune responses important to wound repair (Glaser & Kiecolt-Glaser, 2005). In one study, skin blisters were induced on the forearm. Subjects who reported higher levels of stress produced lower levels of immune proteins necessary for wound healing (Glaser et al., 1999). Stress, then, is not so much the sword that kills the knight, so to speak; rather, it’s the sword that breaks the knight’s shield, and your immune system is that shield.
DIG DEEPER: Stress and Aging: A Tale of Telomeres
Have you ever wondered why people who are stressed often seem to have a haggard look about them? A pioneering study from 2004 suggests that the reason is that stress can actually accelerate the cell biology of aging.
Stress, it seems, can shorten telomeres, which are segments of DNA that protect the ends of chromosomes. Shortened telomeres can inhibit or block cell division, which includes the growth and proliferation of new cells, thereby leading to more rapid aging (Sapolsky, 2004). In the study, researchers compared telomere lengths in the white blood cells in mothers of chronically ill children to those of mothers of healthy children (Epel et al., 2004). Mothers of chronically ill children would be expected to experience more stress than would mothers of healthy children. The longer a mother had spent caring for her ill child, the shorter her telomeres (the correlation between years of caregiving and telomere length was r = -.40). In addition, higher levels of perceived stress were negatively correlated with telomere size (r = -.31). These researchers also found that the average telomere length of the most stressed mothers, compared to the least stressed, was similar to what you would find in people who were 9–17 years older than they were on average.
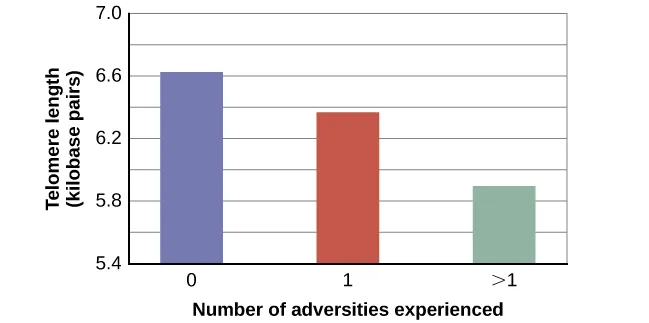
Numerous other studies have continued to find associations between stress and eroded telomeres (Blackburn & Epel, 2012). Some studies have even demonstrated that stress can begin to erode telomeres in childhood and perhaps even before children are born. For example, childhood exposure to violence (e.g., maternal domestic violence, bullying victimization, and physical maltreatment) was found in one study to accelerate telomere erosion from ages 5 to 10 (Shalev et al., 2013). Another study reported that young adults whose mothers had experienced severe stress during their pregnancy had shorter telomeres than those with stress-free and uneventful pregnancies (Entringer et al., 2011). Further, the corrosive effects of childhood stress on telomeres can extend into young adulthood. In an investigation of over 4,000 U.K. women ages 41–80, adverse experiences during childhood (e.g., physical abuse, being sent away from home, and parent divorce) were associated with shortened telomere length (Surtees et al., 2010), and telomere size decreased as the amount of experienced adversity increased (Figure 4.15).
Efforts to dissect the precise cellular and physiological mechanisms linking short telomeres to stress and disease are currently underway. For now, telomeres provide us with yet another reminder that stress, especially during early life, can be just as harmful to our health as smoking or fast food (Blackburn & Epel, 2012).
Cardiovascular Disorders
The cardiovascular system is composed of the heart and blood circulation system. For many years, disorders that involve the cardiovascular system—known as cardiovascular disorders—have been a major focal point in the study of psychophysiological disorders because of the cardiovascular system’s centrality in the stress response (Everly & Lating, 2002). Heart disease is one such condition. Each year, heart disease causes approximately one in three deaths in the United States, and it is the leading cause of death in the developed world (Centers for Disease Control and Prevention [CDC], 2011; Shapiro, 2005).
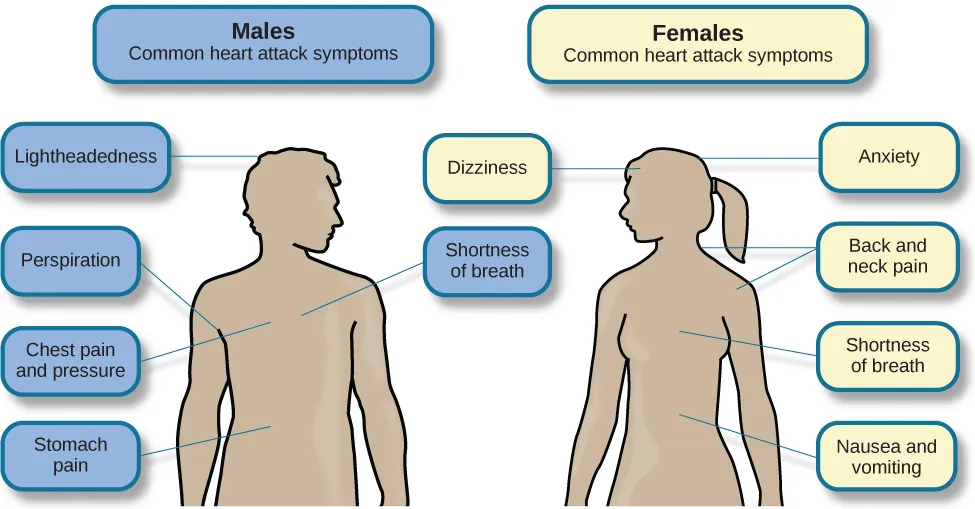
The symptoms of heart disease vary somewhat depending on the specific kind of heart disease one has, but they generally involve angina—chest pains or discomfort that occur when the heart does not receive enough blood (Office on Women’s Health, 2009). The pain often feels like the chest is being pressed or squeezed; burning sensations in the chest and shortness of breath are also commonly reported. Such pain and discomfort can spread to the arms, neck, jaws, stomach (as nausea), and back (American Heart Association [AHA], 2012a) (Figure 14.17).
Hypertension forces a person’s heart to pump harder, thus putting more physical strain on the heart. If left unchecked, hypertension can lead to a heart attack, stroke, or heart failure; it can also lead to kidney failure and blindness. Hypertension is a serious cardiovascular disorder, and it is sometimes called the silent killer because it has no symptoms—one with high blood pressure may not even be aware of it (AHA, 2012b).
Many risk factors contributing to cardiovascular disorders have been identified. These risk factors include social determinants such as aging, income, education, and employment status, as well as behavioral risk factors that include unhealthy diet, tobacco use, physical inactivity, and excessive alcohol consumption; obesity and diabetes are additional risk factors (World Health Organization [WHO], 2013).
Over the past few decades, there has been much greater recognition and awareness of the importance of stress and other psychological factors in cardiovascular health (Nusair, Al-dadah, & Kumar, 2012). Indeed, exposure to stressors of many kinds has also been linked to cardiovascular problems; in the case of hypertension, some of these stressors include job strain (Trudel, Brisson, & Milot, 2010), natural disasters (Saito, Kim, Maekawa, Ikeda, & Yokoyama, 1997), marital conflict (Nealey-Moore, Smith, Uchino, Hawkins, & Olson-Cerny, 2007), and exposure to high traffic noise levels at one’s home (de Kluizenaar, Gansevoort, Miedema, & de Jong, 2007). Perceived discrimination appears to be associated with hypertension among African Americans (Sims et al., 2012). In addition, laboratory-based stress tasks, such as performing mental arithmetic under time pressure, immersing one’s hand in ice water (known as the cold pressor test), mirror tracing, and public speaking, have all been shown to elevate blood pressure (Phillips, 2011).
Our emotions can also influence cardiovascular health. After reviewing and statistically summarizing 35 studies from 1983 to 2006, Chida and Steptoe (2009) concluded that most evidence suggests anger and hostility constitute serious long-term risk factors for adverse cardiovascular outcomes among healthy individuals and those already suffering from heart disease. One reason angry and hostile moods might contribute to cardiovascular diseases is that such moods can create social strain, mainly in the form of antagonistic social encounters with others. This strain could lay the foundation for disease-promoting cardiovascular responses among hostile individuals (Vella, Karmarck, Flory, & Manuck, 2012). In this transactional model, hostility and socials train form a cycle (Figure 4.18).
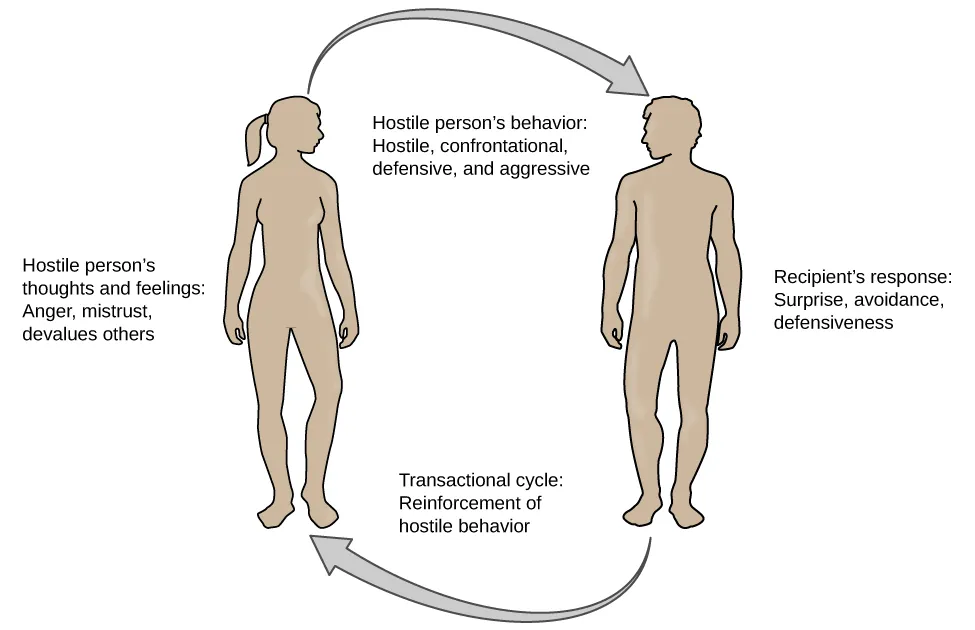
For example, suppose Kaitlin has a hostile disposition; she has a cynical, distrustful attitude toward others and often thinks other people are out to get her. She is very defensive around people, even those she has known for years, and she always looks for signs that others are disrespecting or belittling her. In the shower each morning before work, she often mentally rehearses what she would say to someone who said or did something that angered her, such as making a political statement countering her ideology. As Kaitlin goes through these mental rehearsals, she often grins and thinks about the retaliation on anyone who will irk her that day.
Socially, she is confrontational and tends to use a harsh tone with people, often leading to very disagreeable and sometimes argumentative social interactions. As you might imagine, Kaitlin is not especially popular with others, including coworkers, neighbors, and even members of her own family. They either avoid her at all costs or snap back at her, which causes Kaitlin to become even more cynical and distrustful of others, making her disposition even more hostile. Kaitlin’s hostility—through her own doing—has created an antagonistic environment that cyclically causes her to become even more hostile and angry, potentially setting the stage for cardiovascular problems.
In addition to anger and hostility, a number of other negative emotional states have been linked with heart disease, including negative affectivity and depression (Suls & Bunde, 2005). Negative affectivity is a tendency to experience distressed emotional states involving anger, contempt, disgust, guilt, fear, and nervousness (Watson, Clark, & Tellegen, 1988). It has been linked with the development of both hypertension and heart disease. For example, over 3,000 healthy participants in one study were tracked longitudinally for up to 22 years. Those with higher levels of negative affectivity when the study began, were substantially more likely to develop and be treated for hypertension during the ensuing years than those with lower levels of negative affectivity (Jonas & Lando, 2000). In addition, a study of over 10,000 middle-aged London-based civil servants who were followed an average of 12.5 years revealed that those who earlier had scored in the upper third on a test of negative affectivity were 32% more likely to have experienced heart disease, heart attack, or angina over a period of years than were those who scored in the lowest third (Nabi, Kivimaki, De Vogli, Marmot, & Singh-Manoux, 2008). Hence, negative affectivity appears to be a potentially vital risk factor for the development of cardiovascular disorders.
Depression and the Heart
For centuries, poets and folklore have asserted that there is a connection between moods and the heart (Glassman & Shapiro, 1998). You are undoubtedly familiar with the notion of a broken heart following a disappointing or depressing event and have encountered that notion in songs, films, and literature.
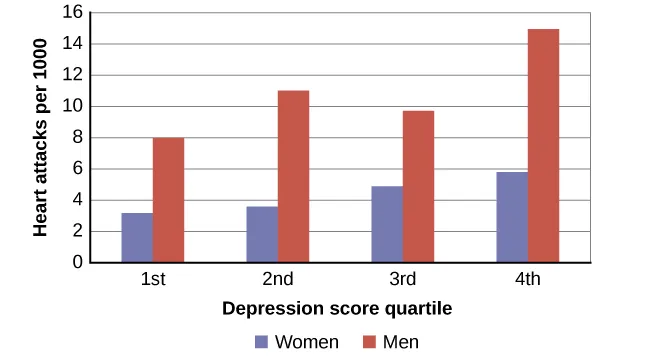
Perhaps the first to recognize the link between depression and heart disease was Benjamin Malzberg (1937), who found that the death rate among institutionalized patients with melancholia (an archaic term for depression) was six times higher than that of the population. A classic study in the late 1970s looked at over 8,000 people diagnosed with manic-depressive disorder (now classified as bipolar disorder) in Denmark, finding a nearly 50% increase in deaths from heart disease among these patients compared with the general Danish population (Weeke, 1979). By the early 1990s, evidence began to accumulate, showing that depressed individuals who were followed for long periods of time were at increased risk for heart disease and cardiac death (Glassman, 2007). In one investigation of over 700 Denmark residents, those with the highest depression scores were 71% more likely to have experienced a heart attack than those with lower depression scores (Barefoot & Schroll, 1996). Figure 14.20 illustrates the gradation in risk of heart attacks for both men and women.
After more than two decades of research, it is now clear that a relationship exists: Patients with heart disease have more depression than the general population, and people with depression are more likely to eventually develop heart disease and experience higher mortality than those who do not have depression (Hare, Toukhsati, Johansson, & Jaarsma, 2013); the more severe the depression, the higher the risk (Glassman, 2007). Consider the following:
- In one study, death rates from cardiovascular problems were substantially higher in depressed people; depressed men were 50% more likely to have died from cardiovascular problems, and depressed women were 70% more likely (Ösby, Brandt, Correia, Ekbom, & Sparén, 2001).
- A statistical review of ten longitudinal studies involving initially healthy individuals revealed that those with elevated depressive symptoms have, on average, a 64% greater risk of developing heart disease than those with fewer symptoms (Wulsin & Singal, 2003).
- A study of over 63,000 registered nurses found that those with more depressive symptoms when the study began were 49% more likely to experience fatal heart disease over a 12-year period (Whang et al., 2009).
The American Heart Association, fully aware of the established importance of depression in cardiovascular diseases, several years ago recommended routine depression screening for all heart disease patients (Lichtman et al., 2008). Recently, they have recommended including depression as a risk factor for heart disease patients (AHA, 2014).
Although the exact mechanisms through which depression might produce heart problems have not been fully clarified, a recent investigation examining this connection in early life has shed some light. In an ongoing study of childhood depression, adolescents who had been diagnosed with depression as children were more likely to be obese, smoke, and be physically inactive than those who had not received this diagnosis (Rottenberg et al., 2014). One implication of this study is that depression, especially if it occurs early in life, may increase the likelihood of living an unhealthy lifestyle, thereby predisposing people to an unfavorable cardiovascular disease risk profile.
It is important to point out that depression may be just one piece of the emotional puzzle in elevating the risk for heart disease and that chronically experiencing several negative emotional states may be especially important. A longitudinal investigation of Vietnam War veterans found that depression, anxiety, hostility, and anger independently predicted the onset of heart disease (Boyle, Michalek, & Suarez, 2006). However, when each negative psychological attribute was combined into a single variable, this new variable (which researchers called psychological risk factor) predicted heart disease more strongly than any of the individual variables. Thus, rather than examining the predictive power of isolated psychological risk factors, it seems crucial for future researchers to examine the effects of combined and more general negative emotional and psychological traits in the development of cardiovascular illnesses.
Headaches
A headache is a continuous pain anywhere in the head and neck region. Inflammation of the sinuses caused by an infection or allergic reaction can cause sinus headaches, which are experienced as pain in the cheeks and forehead. Migraine headaches are a type of headache thought to be caused by blood vessel swelling and increased blood flow (McIntosh, 2013). Migraines are characterized by severe pain on one or both sides of the head, an upset stomach, and disturbed vision. Women more frequently experience them than men (American Academy of Neurology, 2014). Tension headaches are triggered by the tightening/tensing of facial and neck muscles; they are the most commonly experienced headache, accounting for about 42% of all headaches worldwide (Stovner et al., 2007). In the United States, well over one-third of the population experiences tension headaches each year, and 2–3% of the population suffers from chronic tension headaches (Schwartz, Stewart, Simon, & Lipton, 1998).
A number of factors can contribute to tension headaches, including sleep deprivation, skipping meals, eye strain, overexertion, muscular tension caused by poor posture, and stress (MedicineNet, 2013). Although there is uncertainty regarding the exact mechanisms through which stress can produce tension headaches, stress has been demonstrated to increase sensitivity to pain (Caceres & Burns, 1997; Logan et al., 2001). In general, tension headache sufferers, compared to non-sufferers, have a lower threshold for and greater sensitivity to pain (Ukestad & Wittrock, 1996), and they report greater levels of subjective stress when faced with a stressor (Myers, Wittrock, & Foreman, 1998). Thus, stress may contribute to tension headaches by increasing pain sensitivity in already-sensitive pain pathways in tension headache sufferers (Cathcart, Petkov, & Pritchard, 2008).
Regulation of Stress
Regulation of Stress Learning Objectives
By the end of this section, you will be able to:
- Define coping and differentiate between problem-focused and emotion-focused coping
- Describe the importance of perceived control in our reactions to stress
- Explain how social support is vital in health and longevity
As we learned in the previous section, stress—especially if it is chronic—takes a toll on our bodies and can have enormously negative health implications. When we experience events in our lives that we appraise as stressful, it is essential that we use effective coping strategies to manage our stress. Coping refers to mental and behavioral efforts that we use to deal with stress-related problems.
Coping Styles
Lazarus and Folkman (1984) distinguished two fundamental kinds of coping: problem-focused coping and emotion-focused coping. In problem-focused coping, one attempts to manage or alter the problem causing one to experience stress (i.e., the stressor). Problem-focused coping strategies are similar to strategies used in everyday problem-solving: they typically involve identifying the problem, considering possible solutions, weighing the costs and benefits of these solutions, and then selecting an alternative (Lazarus & Folkman, 1984). As an example, suppose Bailey receives a midterm notice that they are failing statistics class. If Bailey adopts a problem-focused coping approach to managing their stress, they will be proactive in alleviating the source of the stress. They might contact their professor to discuss what must be done to raise their grade, or they might also decide to set aside two hours daily to study statistics assignments and seek tutoring assistance. A problem-focused approach to managing stress means we actively try to do things to address the problem.
Emotion-focused coping, in contrast, consists of efforts to change or reduce the negative emotions associated with stress. These efforts may include avoiding, minimizing, or distancing oneself from the problem, or positive comparisons with others (“I’m not as bad off as she is”), or seeking something positive in a negative event (“Now that I’ve been fired, I can sleep in for a few days”). In some cases, emotion-focused coping strategies involve reappraisal, whereby the stressor is construed differently (and somewhat self-deceptively) without changing its objective level of threat (Lazarus & Folkman, 1984). For example, a person sentenced to federal prison who thinks, “This will give me a great chance to network with others,” is using reappraisal. If Bailey adopted an emotion-focused approach to managing their midterm deficiency stress, they might watch a comedy movie, play video games, or spend hours on social media to take their mind off the situation. In a certain sense, emotion-focused coping can be thought of as treating the symptoms rather than the actual cause.
While many stressors elicit both kinds of coping strategies, problem-focused coping is more likely to occur when encountering stressors we perceive as controllable, while emotion-focused coping is more likely to predominate when faced with stressors that we believe we are powerless to change (Folkman & Lazarus, 1980). Clearly, emotion-focused coping is more effective in dealing with uncontrollable stressors. For example, the stress you experience when a loved one dies can be overwhelming. You are simply powerless to change the situation, as there is nothing you can do to bring this person back. The most helpful coping response is emotion-focused coping aimed at minimizing the pain of the grieving period.
Fortunately, most stressors we encounter can be modified and controllable to varying degrees. A person who cannot stand her job can quit and look for work elsewhere; a middle-aged divorcee can find another potential partner; the freshman who fails an exam can study harder next time, and a breast lump does not necessarily mean one is fated to die of breast cancer.
Control and Stress
The desire and ability to predict events, make decisions, and affect outcomes—that is, to enact control in our lives—is a basic tenet of human behavior (Everly & Lating, 2002). Albert Bandura (1997) stated that “the intensity and chronicity of human stress is governed largely by perceived control over the demands of one’s life” (p. 262). As described in his statement, our reaction to potential stressors depends to a large extent on how much control we feel we have over such things. Perceived control is our beliefs about our personal capacity to exert influence over and shape outcomes, and it has major implications for our health and happiness (Infurna & Gerstorf, 2014). Extensive research has demonstrated that perceptions of personal control are associated with a variety of favorable outcomes, such as better physical and mental health and greater psychological well-being (Diehl & Hay, 2010). Greater personal control is also associated with lower reactivity to stressors in daily life. For example, researchers in one investigation found that higher levels of perceived control at one point in time were later associated with lower emotional and physical reactivity to interpersonal stressors (Neupert, Almeida, & Charles, 2007).
DIG DEEPER: Learned Helplessness
When we lack a sense of control over the events in our lives, particularly when those events are threatening, harmful, or noxious, the psychological consequences can be profound. In one of the better illustrations of this concept, psychologist Martin Seligman conducted a series of classic experiments in the 1960s (Seligman & Maier, 1967) in which dogs were placed in a chamber where they received electric shocks from which they could not escape. Later, when these dogs were given the opportunity to escape the shocks by jumping across a partition, most failed to even try; they seemed to just give up and passively accept any shocks the experimenters chose to administer. In comparison, dogs who were previously allowed to escape the shocks tended to jump the partition and escape the pain (Figure 4.21).
Seligman believed that the dogs who failed to try to escape the later shocks were demonstrating learned helplessness: They had acquired a belief that they were powerless to do anything learned helplessness about the stimulation they were receiving. Seligman also believed the passivity and lack of initiative the dogs demonstrated was similar to that observed in human depression. Therefore, Seligman speculated that learned helplessness might be an important cause of depression in humans: Humans who experience negative life events that they believe they cannot control may become helpless. As a result, they give up trying to change the situation, and some may become depressed and show a lack of initiative in future situations in which they can control the outcomes (Seligman, Maier, & Geer, 1968).

Seligman and colleagues later reformulated the original learned helplessness model of depression (Abramson, Seligman, & Teasdale, 1978). Their reformulation emphasized attributions (i.e., a mental explanation for why something occurred) that fostered a sense of learned helplessness. For example, suppose a coworker shows up late to work; your belief as to what caused the coworker’s tardiness would be an attribution (e.g., too much traffic, slept too late, or just doesn’t care about being on time).
The reformulated version of Seligman’s study holds that the attributions made for negative life events contribute to depression. Consider the example of a student who performs poorly on a midterm exam. This model suggests that the student will make three kinds of attributions for this outcome: internal vs. external (believing the outcome was caused by his own personal inadequacies or by environmental factors), stable vs. unstable (believing the cause can be changed or is permanent), and global vs. specific (believing the outcome is a sign of inadequacy in most everything versus just this area). Assume that the student makes an internal (“I’m just not smart”), stable (“Nothing can be done to change the fact that I’m not smart”), and global (“This is another example of how lousy I am at everything”) attribution for the poor performance. The reformulated theory predicts that the student would perceive a lack of control over this stressful event and thus be especially prone to developing depression. Indeed, research has demonstrated that people who have a tendency to make internal, global, and stable attributions for bad outcomes tend to develop symptoms of depression when faced with negative life experiences (Peterson & Seligman, 1984). Fortunately, attribution habits can be changed through practice. Training in healthy attribution habits has been shown to make people less vulnerable to depression (Konnikova, 2015).
Seligman’s learned helplessness model has emerged over the years as a leading theoretical explanation for the onset of major depressive disorder. When you study psychological disorders, you will learn more about the latest reformulation of this model—now called hopelessness theory.
People who report higher levels of perceived control view their health as controllable, making it more likely that they will better manage their health and engage in behaviors conducive to good health (Bandura, 2004). Not surprisingly, greater perceived control has been linked to a lower risk of physical health problems, including declines in physical functioning (Infurna, Gerstorf, Ram, Schupp, & Wagner, 2011), heart attacks (Rosengren et al., 2004), and both cardiovascular disease incidence (Stürmer, Hasselbach, & Amelang, 2006) and mortality from cardiac disease (Surtees et al., 2010). In addition, longitudinal studies of British civil servants have found that those in low-status jobs (e.g., clerical and office support staff) in which the degree of control over the job is minimal are considerably more likely to develop heart disease than those with high-status jobs or considerable control over their jobs (Marmot, Bosma, Hemingway, & Stansfeld, 1997).
The link between perceived control and health may provide an explanation for the frequently observed relationship between social class and health outcomes (Kraus, Piff, Mendoza-Denton, Rheinschmidt, & Keltner, 2012). In general, research has found that more affluent individuals experience better health partly because they tend to believe that they can personally control and manage their reactions to life’s stressors (Johnson & Krueger, 2006). Perhaps buoyed by the perceived level of control, individuals of higher social class may be prone to overestimating their influence over particular outcomes. For example, those of higher social class tend to believe that their votes have greater sway on election outcomes than those of lower social class, which may explain higher voting rates in more affluent communities (Krosnick, 1990). Other research has found that a sense of perceived control can protect less affluent individuals from poorer health, depression, and reduced life satisfaction—all of which tend to accompany lower social standing (Lachman & Weaver, 1998).
Taken together, findings from these and many other studies clearly suggest that perceptions of control and coping abilities are important in managing and coping with the stressors we encounter throughout life.
Social Support
The need to form and maintain strong, stable relationships with others is a powerful, pervasive, and fundamental human motive (Baumeister & Leary, 1995). Building strong interpersonal relationships with others helps us establish a network of close, caring individuals who can provide social support in times of distress, sorrow, and fear. Social support can be thought of as the soothing impact of friends, family, and acquaintances (Baron & Kerr, 2003). Social support can take many forms, including advice, guidance, encouragement, acceptance, emotional comfort, and tangible assistance (such as financial help). Thus, other people can be very comforting to us when we are faced with a wide range of life stressors, and they can be extremely helpful in our efforts to manage these challenges. Even in nonhuman animals, species mates can offer social support during times of stress. For example, elephants seem to be able to sense when other elephants are stressed and will often comfort them with physical contact—such as a trunk touch—or an empathetic vocal response (Krumboltz, 2014).
Scientific interest in the importance of social support first emerged in the 1970s when health researchers developed an interest in the health consequences of being socially integrated (Stroebe & Stroebe, 1996). Interest was further fueled by longitudinal studies showing that social connectedness reduced mortality. In one classic study, nearly 7,000 Alameda County, California, residents were followed over nine years. Those who previously indicated that they lacked social and community ties were likelier to die during the follow-up period than those with more extensive social networks. Compared to those with the most social contacts, isolated men and women were 2.3 and 2.8 times more likely to die. These trends persisted even after controlling for various health-related variables, such as smoking, alcohol consumption, self-reported health at the beginning of the study, and physical activity (Berkman & Syme, 1979).
Since the time of that study, social support has emerged as one of the well-documented psychosocial factors affecting health outcomes (Uchino, 2009). A statistical review of 148 studies conducted between 1982 and 2007 involving over 300,000 participants concluded that individuals with stronger social relationships have a 50% greater likelihood of survival than those with weak or insufficient social relationships (Holt-Lunstad, Smith, & Layton, 2010). According to the researchers, the magnitude of the effect of social support observed in this study is comparable with quitting smoking and exceeds many well-known risk factors for mortality, such as obesity and physical inactivity (Figure 4.22).
A number of large-scale studies have found that individuals with low levels of social support are at greater risk of mortality, especially from cardiovascular disorders (Brummett et al., 2001). Further, higher levels of social support have been linked to better survival rates following breast cancer (Falagas et al., 2007) and infectious diseases, especially HIV infection (Lee & Rotheram-Borus, 2001). In fact, a person with high levels of social support is less likely to contract a common cold. In one study, 334 participants completed questionnaires assessing their sociability; these individuals were subsequently exposed to a virus that causes a common cold and monitored for several weeks to see who became ill. Results showed that increased sociability was linearly associated with a decreased probability of developing a cold (Cohen, Doyle, Turner, Alper, & Skoner, 2003).
For many of us, friends are a vital source of social support. But what if you find yourself in a situation in which you have few friends and companions? Many students who leave home to attend and live at college experience drastic reductions in their social support, which makes them vulnerable to anxiety, depression, and loneliness. Social media can sometimes be useful in navigating these transitions (Raney & Troop Gordon, 2012) but might also cause increases in loneliness (Hunt, Marx, Lipson, & Young, 2018). For this reason, many colleges have designed first-year programs, such as peer mentoring (Raymond & Shepard, 2018), that can help students build new social networks. For some people, our families—especially our parents—are a major source of social support.
Social support appears to work by boosting the immune system, especially among people who are experiencing stress (Uchino, Vaughn, Carlisle, & Birmingham, 2012). In a pioneering study, spouses of cancer patients who reported high levels of social support showed indications of better immune functioning on two out of three immune functioning measures compared to spouses who were below the median on reported social support (Baron, Cutrona, Hicklin, Russell, & Lubaroff, 1990). Studies of other populations have produced similar results, including those of spousal caregivers of dementia sufferers, medical students, elderly adults, and cancer patients (Cohen & Herbert, 1996; Kiecolt-Glaser, McGuire, Robles, & Glaser, 2002).
In addition, social support has been shown to reduce blood pressure for people performing stressful tasks, such as giving a speech or performing mental arithmetic (Lepore, 1998). In these kinds of studies, participants are usually asked to perform a stressful task alone, with a stranger present (who may be supportive or unsupportive), or with a friend present. Those tested with a friend present generally exhibit lower blood pressure than those tested alone or with a stranger (Fontana, Diegnan, Villeneuve, & Lepore, 1999). In one study, 112 female participants who performed stressful mental arithmetic exhibited lower blood pressure when they received support from a friend rather than a stranger, but only if the friend was a male (Phillips, Gallagher, & Carroll, 2009). Although these findings are somewhat difficult to interpret, the authors mention that it is possible that females feel less supported and more evaluated by other females, particularly females whose opinions they value.
Taken together, the findings above suggest one of the reasons social support is connected to favorable health outcomes is that it has several beneficial physiological effects in stressful situations. However, it is also important to consider the possibility that social support may lead to better health behaviors, such as a healthy diet, exercising, smoking cessation, and cooperation with medical regimens (Uchino, 2009).
DIG DEEPER: Stress and Discrimination
Being the recipient of prejudice and discrimination is associated with a number of negative outcomes. Many studies have shown how perceived discrimination is a significant stressor for marginalized groups (Pascoe & Smart Richman, 2009). Discrimination negatively impacts both the physical and mental health of individuals in stigmatized groups. As you’ll learn when you study social psychology, various social identities (such as gender, age, religion, sexuality, and ethnicity) often lead people to simultaneously be exposed to multiple forms of discrimination, which can have even stronger negative effects on mental and physical health (Vines, Ward, Cordoba, & Black, 2017). For example, the amplified levels of discrimination faced by Latinx transgender women may have related effects, leading to high stress levels and poor mental and physical health outcomes.
Perceived control and the general adaptation syndrome help explain the process by which discrimination affects mental and physical health. Discrimination can be conceptualized as an uncontrollable, persistent, and unpredictable stressor. When a discriminatory event occurs, the target of the event initially experiences an acute stress response (alarm stage). This acute reaction alone does not typically have a great impact on health. However, discrimination tends to be a chronic stressor. As people in marginalized groups experience repeated discrimination, they develop a heightened reactivity as their bodies prepare to act quickly (resistance stage). This long-term accumulation of stress responses can eventually lead to increased negative emotions and wear on physical health (exhaustion stage). This explains why a history of perceived discrimination is associated with various mental and physical health problems, including depression, cardiovascular disease, and cancer (Pascoe & Smart Richman, 2009).
Protecting stigmatized groups from the negative impact of discrimination-induced stress may involve reducing the incidence of discriminatory behaviors in conjunction with protective strategies that reduce the impact of discriminatory events when they occur. Civil rights legislation has protected some stigmatized groups by making discrimination a prosecutable offense in many social contexts. However, some groups (e.g., transgender people) often lack important legal recourse when discrimination occurs. Moreover, most modern discrimination comes in subtle forms that fall below the radar of the law. For example, discrimination may be experienced as selective inhospitality that the target perceives as race-based discrimination, but little is done in response since it would be easy to attribute the behavior to other causes. Although some cultural changes are increasingly helping people to recognize and control subtle discrimination, such shifts may take a long time.
Similar to other stressors, buffers like social support and healthy coping strategies effectively reduce perceived discrimination’s impact. For example, one study (Ajrouch, Reisine, Lim, Sohn, & Ismail, 2010) showed that discrimination predicted high psychological distress among African American mothers living in Detroit. However, the women with readily available emotional support from friends and family experienced less distress than those with fewer social resources. While coping strategies and social support may buffer the effects of discrimination, they fail to erase all of the negative impacts. Vigilant anti-discrimination efforts, including developing legal protections for vulnerable groups, are needed to reduce discrimination, stress, and the resulting physical and mental health effects.
Stress Reduction Techniques
Beyond having a sense of control and establishing social support networks, there are numerous other means by which we can manage stress (Figure 4.23). A common technique people use to combat stress is exercise (Salmon, 2001). It is well-established that exercise, both of long (aerobic) and short (anaerobic) duration, is beneficial for both physical and mental health (Everly & Lating, 2002). There is considerable evidence that physically fit individuals are more resistant to the adverse effects of stress and recover more quickly from stress than less physically fit individuals (Cotton, 1990). In a study of more than 500 Swiss police officers and emergency service personnel, increased physical fitness was associated with reduced stress, and regular exercise was reported to protect against stress-related health problems (Gerber, Kellman, Hartman, & Pühse, 2010).
Exercise may be beneficial because it might buffer some of the deleterious physiological mechanisms of stress. One study found rats that exercised for six weeks showed a decrease in hypothalamic-pituitary-adrenal responsiveness to mild stressors (Campeau et al., 2010). In high-stress humans, exercise has been shown to prevent telomere shortening, which may explain the common observation of a youthful appearance among those who exercise regularly (Puterman et al., 2010). Further, exercise in later adulthood appears to minimize the detrimental effects of stress on the hippocampus and memory (Head, Singh, & Bugg, 2012). Among cancer survivors, exercise has been shown to reduce anxiety (Speck, Courneya, Masse, Duval, & Schmitz, 2010) and depressive symptoms (Craft, VanIterson, Helenowski, Rademaker, & Courneya, 2012). Clearly, exercise is a highly effective tool for regulating stress.
In the 1970s, Herbert Benson, a cardiologist, developed a stress reduction method called the relaxation response technique (Greenberg, 2006). The relaxation response technique combines relaxation with transcendental meditation and consists of four components (Stein, 2001):
- Sitting upright on a comfortable chair with feet on the ground and body in a relaxed position,
- Being in a quiet environment with eyes closed,
- Repeating a word or a phrase—a mantra—to oneself, such as “alert mind, calm body,”
- Passively allowing the mind to focus on pleasant thoughts, such as nature or the warmth of your blood nourishing your body.
The relaxation response approach is conceptualized as a general approach to stress reduction that reduces sympathetic arousal and has been used effectively to treat people with high blood pressure (Benson & Proctor, 1994).
Another technique to combat stress, biofeedback, was developed by Gary Schwartz at Harvard University in the early 1970s. Biofeedback is a technique that uses electronic equipment to measure a person’s neuromuscular and autonomic activity—feedback is provided in the form of visual or auditory signals. The main assumption of this approach is that providing somebody with biofeedback will enable the individual to develop strategies that help gain some level of voluntary control over what are normally involuntary bodily processes (Schwartz & Schwartz, 1995). A number of different bodily measures have been used in biofeedback research, including facial muscle movement, brain activity, and skin temperature, and it has been applied successfully with individuals experiencing tension headaches, high blood pressure, asthma, and phobias (Stein, 2001).
Stress Crossword
Sexual Health and Gender Identity
Sexual Health and Gender Identity Learning Objectives
By the end of this section, you will be able to:
- Understand basic biological mechanisms regulating sexual behavior and motivation
- Appreciate the importance of Alfred Kinsey’s research on human sexuality
- Recognize the contributions that William Masters and Virginia Johnson’s research made to our understanding of the sexual response cycle
- Define sexual orientation and gender identity
- Identify biopsychosocial factors impacting sexual desire and normal sexual functioning
Sex is an important part of our lives. From an evolutionary perspective, the reason is obvious—the perpetuation of the species. Sexual behavior in humans, however, involves much more than reproduction. This section provides an overview of research that has been conducted on human sexual behavior and motivation. This section will close with a discussion of issues related to gender and sexual orientation.
Physiological Mechanisms of Sexual Behavior and Motivation

Much of what we know about the physiological mechanisms that underlie sexual behavior and motivation comes from animal research. As you’ve learned, the hypothalamus plays an important role in motivated behaviors, and sex is no exception. In fact, lesions to an area of the hypothalamus called the medial preoptic area completely disrupt a male rat’s ability to engage in sexual behavior. Surprisingly, medial preoptic lesions do not change how hard a male rat is willing to work to gain access to a sexually receptive female (Figure 4.24). This suggests that the ability to engage in sexual behavior and the motivation to do so may be mediated by neural systems distinct from one another.
Animal research suggests that limbic system structures such as the amygdala and nucleus accumbens are especially important for sexual motivation. Damage to these areas results in a decreased motivation to engage in sexual behavior while leaving the ability to do so intact (Figure 4.25; Everett, 1990). Similar dissociations of sexual motivation and sexual ability have also been observed in the female rat (Becker, Rudick, & Jenkins, 2001; Jenkins & Becker, 2001).
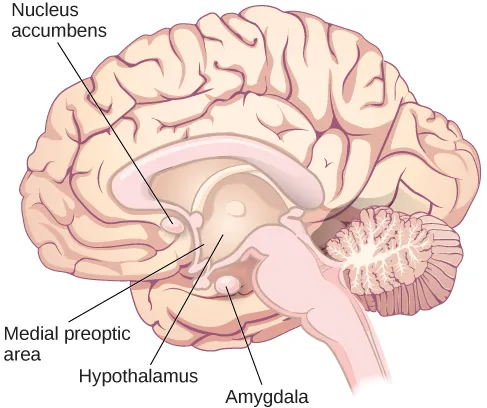
Although human sexual behavior is much more complex than that seen in rats, some parallels between animals and humans can be drawn from this research. The worldwide popularity of drugs used to treat erectile dysfunction (Conrad, 2005) shows that sexual motivation and the ability to engage in sexual behavior can also be dissociated in humans. Moreover, disorders that involve abnormal hypothalamic function are often associated with hypogonadism (reduced function of the gonads) and reduced sexual function (e.g., Prader-Willi syndrome). Given the hypothalamus’s role in endocrine function, it is unsurprising that hormones secreted by the endocrine system also play important roles in sexual motivation and behavior. For example, many animals show no sign of sexual motivation in the absence of the appropriate combination of sex hormones from their gonads. While this is not the case for humans, there is considerable evidence that sexual motivation for both men and women varies as a function of circulating testosterone levels (Bhasin, Enzlin, Coviello, & Basson, 2007; Carter, 1992; Sherwin, 1988).
Kinsey’s Research
Before the late 1940s, access to reliable, empirically-based information on sex was limited. Physicians were considered authorities on all issues related to sex, despite the fact that they had little to no training in these issues, and it is likely that most of what people knew about sex had been learned either through their own experiences or by talking with their peers. Convinced that people would benefit from a more open dialogue on issues related to human sexuality, Dr. Alfred Kinsey of Indiana University initiated large-scale survey research on the topic (Figure 4.26). The results of some of these efforts were published in two books—Sexual Behavior in the Human Male and Sexual Behavior in the Human Female—which were published in 1948 and 1953, respectively (Bullough, 1998).

At the time, the Kinsey reports were quite sensational. Never before had the American public seen its private sexual behavior become the focus of scientific scrutiny on such a large scale. The books, which were filled with statistics and scientific lingo, sold remarkably well to the general public, and people began to engage in open conversations about human sexuality. As you might imagine, not everyone was happy that this information was being published. In fact, these books were banned in some countries. Ultimately, the controversy resulted in Kinsey losing funding that he had secured from the Rockefeller Foundation to continue his research efforts (Bancroft, 2004).
Although Kinsey’s research has been widely criticized as being riddled with sampling and statistical errors (Jenkins, 2010), there is little doubt that this research was very influential in shaping future research on human sexual behavior and motivation. Kinsey described a remarkably diverse range of sexual behaviors and experiences reported by the volunteers participating in his research. Behaviors that had once been considered exceedingly rare or problematic were demonstrated to be much more common and innocuous than previously imagined (Bancroft, 2004; Bullough, 1998).
Among the results of Kinsey’s research were the findings that women are as interested and experienced in sex as their male counterparts, that both males and females masturbate without adverse health consequences, and that homosexuality was fairly common (Bancroft, 2004). Kinsey also developed a continuum known as the Kinsey scale that is still commonly used today to categorize an individual’s sexual orientation (Jenkins, 2010). According to that scale, sexual orientation is an individual’s emotional and erotic attraction to same-sexed individuals (homosexual), opposite-sexed individuals (heterosexual), or both (bisexual).
Masters and Johnson’s Research
In 1966, William Masters and Virginia Johnson published a book detailing the results of their observations of nearly 700 people who agreed to participate in their study of physiological responses during sexual behavior. Unlike Kinsey, who used personal interviews and surveys to collect data, Masters and Johnson observed people having intercourse in various positions, and they observed people masturbating, manually or with the aid of a device. While this was occurring, researchers recorded measurements of physiological variables, such as blood pressure and respiration rate, as well as measurements of sexual arousal, such as vaginal lubrication and penile tumescence (swelling associated with an erection). In total, Masters and Johnson observed nearly 10,000 sexual acts as a part of their research (Hock, 2008).
Based on these observations, Masters and Johnson divided the sexual response cycle into four phases that are fairly similar in men and women: excitement, plateau, orgasm, and resolution (Figure 4.27). The excitement phase is the arousal phase of the sexual response cycle, and it is marked by the erection of the penis or clitoris and lubrication and expansion of the vaginal canal. During plateau, women experience further swelling of the vagina and increased blood flow to the labia minora, and men experience full erection and often exhibit pre-ejaculatory fluid. Both men and women experience increases in muscle tone during this time. Orgasm is marked in women by rhythmic contractions of the pelvis and uterus and increased muscle tension. In men, pelvic contractions are accompanied by a buildup of seminal fluid near the urethra that is ultimately forced out by contractions of genital muscles (i.e., ejaculation). Resolution is the relatively rapid return to an unaroused state accompanied by a decrease in blood pressure and muscular relaxation. While many women can quickly repeat the sexual response cycle, men must pass through a longer refractory period as part of resolution. The refractory period is a period of time that follows an orgasm during which an individual is incapable of experiencing another orgasm. In men, the duration of the refractory period can vary dramatically from individual to individual, with some refractory periods as short as several minutes and others as long as a day. As men age, their refractory periods tend to span longer periods of time.
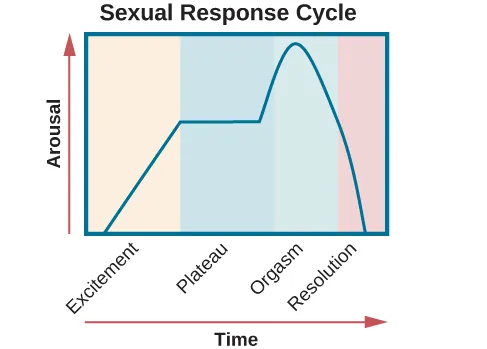
In addition to the insights that their research provided with regard to the sexual response cycle and the multi-orgasmic potential of women, Masters and Johnson also collected important information about reproductive anatomy. Their research demonstrated the often cited statistic of the average size of a flaccid and an erect penis (3 and 6 inches, respectively) as well as dispelling long-held beliefs about relationships between the size of a man’s erect penis and his ability to provide sexual pleasure to his female partner. Furthermore, they determined that the vagina is a very elastic structure that can conform to penises of various sizes (Hock, 2008).
Sexual Orientation

As mentioned earlier, a person’s sexual orientation is their emotional, sexual, or romantic attraction toward another individual (Figure 4.28). While many people identify as heterosexual, a sizable population of people within the United States identify as homosexual, bisexual, pansexual, asexual, or other non-hetero sexualities. Research suggests that somewhere between 3% and 10% of the population identifies as homosexual (Kinsey, Pomeroy, & Martin, 1948; LeVay, 1996; Pillard & Bailey, 1995). (Bisexual people are attracted to people of their own gender and another gender; pansexual people experience attraction without regard to sex, gender identity, or gender expression; asexual people do not experience sexual attraction or have little or no interest in sexual activity.)
Issues of sexual orientation have long fascinated scientists interested in determining what predicts sexual orientation. For many years, people believed these differences arose from different socialization and familial experiences. However, research has consistently demonstrated that family backgrounds and experiences are very similar among heterosexuals and sexual minorities (Bell, Weinberg, & Hammersmith, 1981; Ross & Arrindell, 1988).
Genetic and biological mechanisms have also been proposed, and the balance of research evidence suggests that sexual orientation has an underlying biological component. For instance, over the past 25 years, research has demonstrated gene-level contributions to sexual orientation (Bailey & Pillard, 1991; Hamer, Hu, Magnuson, Hu, & Pattatucci, 1993; Rodriguez-Larralde & Paradisi, 2009), with some researchers estimating that genes account for at least half of the variability seen in human sexual orientation (Pillard & Bailey, 1998). Other studies report differences in brain structure and function (Allen & Gorski, 1992; Byne et al., 2001; Hu et al., 2008; LeVay, 1991; Ponseti et al., 2006; Rahman & Wilson, 2003a; Swaab & Hofman, 1990), and even differences in basic body structure and function have been observed (Hall & Kimura, 1994; Lippa, 2003; Loehlin & McFadden, 2003; McFadden & Champlin, 2000; McFadden & Pasanen, 1998; Rahman & Wilson, 2003b). In aggregate, the data suggest that, to a significant extent, sexual orientations are something we are born with.
Misunderstandings About Sexual Orientation
Regardless of how sexual orientation is determined, research has made clear that sexual orientation is not a choice, but rather it is a relatively stable characteristic of a person that cannot be changed. Claims of successful conversion therapy have received wide criticism from the research community due to significant concerns with research design, recruitment of experimental participants, and interpretation of data. As such, there is no credible scientific evidence to suggest that individuals can change their sexual orientation (Jenkins, 2010).
Dr. Robert Spitzer, the author of one of the most widely-cited examples of successful conversion therapy, apologized to both the scientific community and the gay community for his mistakes, and he publically recanted his own paper in a public letter addressed to the editor of Archives of Sexual Behavior in the spring of 2012 (Carey, 2012). In this letter, Spitzer wrote,
I was considering writing something that would acknowledge that I now judge the major critiques of the study as largely correct. . . . I believe I owe the gay community an apology for my study making unproven claims of the efficacy of reparative therapy. I also apologize to any gay person who wasted time or energy undergoing some form of reparative therapy because they believed that I had proven that reparative therapy works with some “highly motivated” individuals. (Becker, 2012, pars. 2, 5)
Citing research that suggests not only that gay conversion therapy is ineffective but also potentially harmful, legislative efforts to make such therapy illegal have either been enacted (e.g., it is now illegal in California) or are underway across the United States, and many professional organizations have issued statements against this practice (Human Rights Campaign, n.d.)
Gender Identity
Many people conflate sexual orientation with gender identity because of stereotypical attitudes that exist about gay and lesbian sexuality. In reality, these are two related but different issues. Gender identity refers to one’s sense of gender which is not confined to the gender binary of male or female. When individuals do not feel comfortable identifying with the gender associated with their biological sex, they experience gender dysphoria. Gender dysphoria is a diagnostic category in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) that describes individuals who have a gender identity different than their biological sex. This dysphoria must persist for at least six months and result in significant distress or dysfunction to meet DSM-5 diagnostic criteria.

Many people who have gender dysphoria seek to live their lives in ways that are consistent with their own gender identity. This might involve dressing in gender-affirming clothing. These individuals may also undertake transgender hormone therapy in an attempt to make their bodies look more like the opposite sex, and in some cases, they elect to have surgeries to alter the appearance of their external genitalia to resemble that of their gender identity (Figure 10.19).
Our scientific knowledge and a general understanding of gender identity continue to evolve, and young people today have more opportunities to explore and openly express different ideas about what gender means than previous generations. Recent studies indicate that the majority of young adults (those ages 18–34) regard gender as a spectrum instead of a strict male/female binary and that 12% identify as transgender or gender non-conforming. Additionally, over half of people ages 13–20 know people who use gender-neutral pronouns (such as they/them) (Kennedy, 2017). As young people lead this change, other changes are emerging in various spheres, from public bathroom policies to retail organizations. For example, some retailers are starting to change traditional gender-based marketing of products, such as removing “pink and blue” clothing and toy aisles. Even with these changes, those who exist outside of traditional gender norms face difficult challenges. Even people who vary slightly from traditional norms can be the target of discrimination and sometimes even violence.
Cultural Factors in Sexual Orientation and Gender Identity
Sociocultural factors very much influence issues related to sexual orientation and gender identity. Even the ways in which we define sexual orientation, and gender vary from one culture to the next. While in the United States, heterosexuality has historically been viewed as the norm, there are societies that have different attitudes regarding gay behavior. In fact, in some instances, periods of exclusively homosexual behavior are socially prescribed as a part of normal development and maturation. For example, in parts of New Guinea, young boys are expected to engage in sexual behavior with other boys for a given period of time because it is believed that doing so is necessary for these boys to become men (Baldwin & Baldwin, 1989).
There has historically been a two-gendered culture in the United States. We have tended to classify an individual as either male or female. However, in some cultures, there are additional gender variants resulting in more than two gender categories. For example, in Thailand, you can be male, female, or kathoey. A kathoey is an individual who would be described as intersexed or transgender in the United States (Tangmunkongvorakul, Banwell, Carmichael, Utomo, & Sleigh, 2010). Intersex is a broad term referring to people whose bodies are not strictly biologically male or female (Hughes et al., 2006). Intersex conditions can present at any time during life (Creighton, 2001). Sometimes a child may be born with components of male and female genitals, and other times XY chromosomal differences are present (Creighton, 2001; Hughes et al., 2006).
DIG DEEPER: The Case of David Reimer
In August of 1965, Janet and Ronald Reimer of Winnipeg, Canada, welcomed the birth of their twin sons, Bruce and Brian. Within a few months, the twins were experiencing urinary problems; doctors recommended the problems could be alleviated by having the boys circumcised. A malfunction of the medical equipment used to perform the circumcision resulted in Bruce’s penis being irreparably damaged. Distraught, Janet and Ronald looked to expert advice on what to do with their baby boy. By happenstance, the couple became aware of Dr. John Money at Johns Hopkins University and his theory of psychosexual neutrality (Colapinto, 2000).
Dr. Money had spent a considerable amount of time researching transgender individuals and individuals born with ambiguous genitalia. As a result of this work, he developed a theory of psychosexual neutrality. His theory asserted that we are essentially neutral at birth with regard to our gender identity and that we don’t assume a concrete gender identity until we begin to master language. Furthermore, Dr. Money believed that the way in which we are socialized in early life is ultimately much more important than our biology in determining our gender identity (Money, 1962).
Dr. Money encouraged Janet and Ronald to bring the twins to Johns Hopkins University, and he convinced them that they should raise Bruce as a girl. Left with few other options at the time, Janet and Ronald agreed to have Bruce’s testicles removed and to raise him as a girl. When they returned home to Canada, they brought with them Brian and his “sister,” Brenda, along with specific instructions to never reveal to Brenda that she had been born a boy (Colapinto, 2000).
Early on, Dr. Money shared with the scientific community the great success of this natural experiment that seemed to fully support his theory of psychosexual neutrality (Money, 1975). Indeed, in early interviews with the children, it appeared that Brenda was a typical little girl who liked to play with “girly” toys and do “girly” things.
However, Dr. Money was less than forthcoming with information that seemed to argue against the success of the case. In reality, Brenda’s parents were constantly concerned that their little girl wasn’t really behaving as most girls did, and by the time Brenda was nearing adolescence, it was painfully obvious to the family that she was really having a hard time identifying as a female. In addition, Brenda was becoming increasingly reluctant to continue her visits with Dr. Money to the point that she threatened suicide if her parents made her go back to see him again.
At that point, Janet and Ronald disclosed the true nature of Brenda’s early childhood to their daughter. While initially shocked, Brenda reported that things made sense to her now, and ultimately, by the time she was an adolescent, Brenda had decided to identify as a male. Thus, she became David Reimer.
David was quite comfortable in his masculine role. He made new friends and began to think about his future. Although his castration had left him infertile, he still wanted to be a father. In 1990, David married a single mother and loved his new role as a husband and father. In 1997, David was made aware that Dr. Money was continuing to publicize his case as a success supporting his theory of psychosexual neutrality. This prompted David and his brother to go public with their experiences in attempt to discredit the doctor’s publications. While this revelation created a firestorm in the scientific community for Dr. Money, it also triggered a series of unfortunate events that ultimately led to David dying by suicide in 2004 (O’Connell, 2004).
This sad story speaks to the complexities involved in gender identity. While the Reimer case had earlier been paraded as a hallmark of how socialization trumped biology in terms of gender identity, the truth of the story made the scientific and medical communities more cautious in dealing with cases that involve intersex children and how to deal with their unique circumstances. In fact, stories like this one have prompted measures to prevent unnecessary harm and suffering to children who might have issues with gender identity. For example, in 2013, a law took effect in Germany, allowing parents of intersex children to classify their children as indeterminate so that children can self-assign the appropriate gender once they have fully developed their own gender identities (Paramaguru, 2013).
Chapter Quiz
Chapter Summary
4.1 Biological Rhythms and Sleep
- Our sleep-wake cycle, an example of a circadian rhythm, is regulated by the light-dark cycle in our environment. This means that when the sun rises, and more light is present, we are awake and tend to fall asleep when the sun sets.
- Electronic screens at night, jet lag, and light night working shifts can disrupt our circadian rhythm, which leads to many negative health effects.
- It is possible for people to have different circadian rhythms called chronotypes, which results in certain people naturally waking up early, and others staying awake late into the night.
4.2 Sleep and Why We Sleep
- The suprachiasmatic nucleus regulates our circadian rhythm, the thalamus regulates slow-wave sleep, and the pons regulates REM sleep.
- The pituitary gland releases hormones during sleep, including melatonin, follicle-stimulating hormone (FSH), luteinizing hormone (LH), and growth hormone.
- Describe several theories aimed at explaining the function of sleep.
- Adaptive theories of sleep are evolutionary-based and suggest that we sleep to restore the energy used during the day and protect ourselves against predators. However, the evidence supporting this theory is lacking.
- A more evidence-supported theory is the cognitive function of sleep. Sleep allows our brain to form strong memories, increases creative thinking, and improves decision-making and logical thinking skills.
4.3 Stages of Sleep
- Non-REM sleep can be broken down into three stages which prepare us for REM sleep and are characterized by their unique brainwave activity.
- Non-REM stage 3 sleep is also known as slow-wave sleep.
- REM sleep has brain activity similar to what happens when we are awake, and this is the stage where dreams happen
- REM sleep is especially important for emotion processing and regulation
- The National Sleep Foundation has set recommendations for the hours of sleep we need. Babies need the most sleep, and the required hours decrease as we age. For college-aged students, they recommend 7-9 hours of sleep per night.
- Sleep debt occurs when we have a sleep deficit.
- Sleep deprivation has many negative physiological, cognitive, and psychological consequences, including depression, blood pressure, stress, and decreased immune functioning.
4.4 Sleep Problems and Disorders
- Insomnia is a sleep disorder marked by difficulty falling or staying asleep and is associated with higher chances of developing anxiety or depressive disorders.
- Parasomnias are disruptive sleep-related disorders, including sleepwalking, in which involuntary motor activity occurs during sleep, and restless leg syndrome, where uncomfortable sensations in the legs prevent the individuals from falling or staying asleep.
- Narcolepsy is a sleep disorder marked by uncontrollably falling asleep at inopportune times throughout the day. Treatment is typically stimulant drugs that can increase brain activity and keep the individual awake during the day.
14.1 What is Stress?
- Our sympathetic nervous system is activated when we encounter stressful situations, triggering our fight-or-flight response. The HPA axis is also activated, and brain system pathways release cortisol, the stress hormone.
- The general adaptation syndrome describes our body’s response to stress in three stages: alarm, resistance, and exhaustion.
- Chronic stressors persist for long periods, such as long-term unemployment and imprisonment.
- Acute stressors are brief stressful events such as arguments, breaking a bone, and losing your phone.
- Eustress is a beneficial stress type that can result from positive events such as a wedding or a new job.
14.3 Stress and Illness
- Sometimes stress can be so severe and chronic that it leads to or worsens physical disorders, called psychophysiological disorders. An example is hypertension which is increased blood pressure due to stress.
- The immune system protects us from disease and getting infections. High levels of stress that are chronic can decrease immune functioning. This makes us more susceptible to getting sick.
- Because of the cardiovascular response of the sympathetic nervous system activation, when we are constantly stressed, it can increase the likelihood of developing cardiovascular problems. Although the increased blood pressure and breathing rate are advantageous to help us escape danger, it is detrimental to our health at inappropriate times.
14.4 Regulation of Stress
- Problem-focused coping seeks to eliminate the stressor at the source and is more direct.
- Emotion-focused coping seeks to alleviate the emotional distress caused by the stressor, which can sometimes lead to avoidance of the stressor.
- Greater perceived control over our stressors leads to a decreased stress response.
- Less perceived control can lead to learned helplessness, characterized by hopelessness and decreased motivation.
- Social support from our friends and family leads to more successful management of stressful situations since they can provide comfort and support.
10.3 Sexual Health and Gender Identity
- The hypothalamus, amygdala, and nucleus accumbens are important for sexual motivation.
- The hypothalamus specifically triggers the release of hormones that influence sexual motivation and behavior.
- Kinsey’s research, because of its topic and content, began to increase the discussion of sex, and sexual behaviors, contributing to decreased stigma surrounding the subject. He also developed a scale that categorizes an individual’s sexual orientation.
- Masters and Johnson’s research defined the sexual response cycle as consisting of four distinct stages: excitement, plateau, orgasm, and resolution. They also examined differences in these stages by age and by biological sex.
- Sexual orientation describes our attraction patterns, including romantic, sexual, and emotional. Examples of sexual orientations include heterosexuality, homosexuality, pansexuality, bisexuality, and asexuality.
- Gender identity describes our beliefs surrounding our gender. It is important to recognize that the gender binary of male and female does not accurately capture the complexity of gender. Individuals can also identify as non-binary, gender fluid, or transgender.
- Sociocultural factors heavily influence sexual orientation and gender identity since culture can determine “normal” or socially acceptable behaviors. In other countries with cultural differences from the West, they may recognize more gender identities or be more inclusive of certain sexual orientations.
a biological rhythm that takes place over a period of about 24 hours
state of equilibrium—biological conditions, such as body temperature, are maintained at optimal levels
A hormone thought to be involved in the regulation of various biological rhythms and of the immune system during sleep
individual differences in circadian patterns of activity
the brain’s control of switching between sleep and wakefulness as well as coordinating this cycle with the outside world
a collection of symptoms that results from the mismatch between our internal circadian cycles and our environment
a sleep-deprived individual will fall asleep more quickly during subsequent opportunities for sleep
Relatively low frequency (8–13Hz), and high amplitude patterns of electrical activity (waves), which are present during non-REM stage 1 sleep
Low frequency (4–7 Hz) waves with higher amplitude than alpha waves that emerge during non-REM stage 1 sleep and dominate non-REM stage 2 sleep.
rapid bursts of higher-frequency brain waves that may be important for learning and memory
a very high amplitude pattern of brain activity that may in some cases occur in response to environmental stimuli
low frequency (less than 3 Hz), and high amplitude brain waves that emerge during non-REM stage 3 sleep
If people are deprived of REM sleep and then allowed to sleep without disturbance, they will spend more time in REM sleep in what would appear to be an effort to recoup the lost time in REM
the actual content, or storyline, of a dream
the hidden meaning of a dream which requires interpretation
insufficient amount of sleep over a number of days which leads to a deficit
A sleep disorder characterized by a consistent difficulty in falling or staying asleep
Occurs when an individual engages in relatively complex behaviors while sleeping such as wandering about or driving a car. Most common during slow-wave sleep
a sense of panic during sleep often accompanied by screams and attempts to escape from the immediate environment
A sleep disorder characterized by involuntarily falling asleep at inopportune times
a stress hormone that helps provide that boost of energy when we first encounter a stressor, preparing us to run away or fight
Stressful events that persist over an extended period of time
Brief focal events that sometimes continue to be experienced as overwhelming well after the event has ended
A normal or moderate stressor that can be beneficial rather than harmful
Physical disorders or diseases whose symptoms are brought about or worsened by stress and emotional factors
The study of how psychological factors such as stress influence the immune system and immune functioning
a type of chest pain or discomfort that occur when the heart does not receive enough blood
A cardiovascular disorder characterized by high blood pressure. Known as "the silent killer."
a tendency to experience distressed emotional states involving anger, contempt, disgust, guilt, fear, and nervousness
a continuous pain anywhere in the head and neck region
a type of headache thought to be caused by blood vessel swelling, and increased blood, characterized by severe pain on one or both sides of the head, an upset stomach, and disturbed vision
one attempts to manage or alter the problem causing one to experience stress (i.e., the stressor)
efforts to change or reduce the negative emotions associated with stress
our beliefs about our personal capacity to exert influence over and shape outcomes, and it has major implications for our health and happiness
The perceived belief of powerlessness when repeated attempts to avoid an aversive stimulus fail. May be a important cause of depression in humans
The soothing impact of friends, family, and acquaintances, for example, advice, guidance, encouragement, acceptance, emotional comfort, and tangible assistance
a technique that uses electronic equipment to measure a person’s neuromuscular and autonomic activity—feedback is provided in the form of visual or auditory signals
A condition characterized by reduced function of the gonads
An individual's patterns of sexual attraction— including homosexuality, heterosexuality, bisexuality, pansexuality, and asexuality. Sexual orientation often correlates with romantic attraction
the arousal phase of the sexual response cycle, marked by the erection of the penis or clitoris and lubrication and expansion of the vaginal canal
The second phase of the sexual response cycle. Women experience further swelling of the vagina and increased blood flow to the labia minora, and men experience full erection and often exhibit pre-ejaculatory fluid
The third phase of the sexual response cycle. It is marked in women by rhythmic contractions of the pelvis and uterus and increased muscle tension. In men, pelvic contractions are accompanied by a buildup of seminal fluid near the urethra that is ultimately forced out by contractions of genital muscles (i.e., ejaculation)
The final phase of the sexual response cycle. The relatively rapid return to an unaroused state accompanied by a decrease in blood pressure and muscular relaxation
a period of time that follows an orgasm during which an individual is incapable of experiencing another orgasm
How people cognitively identify regarding gendered schemas, for example male, female, non-binary, or genderfluid identity.
a broad term referring to people whose bodies are not strictly biologically male or female

