12 Psychological Disorders
On Monday, September 16, 2013, a gunman killed 12 people as the workday began at the Washington Navy Yard in Washington, DC. Aaron Alexis, 34, had a troubled history: he thought that he was being controlled by radio waves. He called the police to complain about voices in his head and being under surveillance by “shadowy forces” (Thomas, Levine, Date, & Cloherty, 2013). While Alexis’s actions cannot be excused, it is clear that he had some form of mental illness. Mental illness is not necessarily a cause of violence; it is far more likely that the mentally ill will be victims rather than perpetrators of violence (Stuart, 2003). If, however, Alexis had received the help he needed, this tragedy might have been averted.
Table of Contents
15.1 What Are Psychological Disorders?
15.2 Diagnosing and Classifying Psychological Disorders
15.3 Anxiety Disorders
15.4 Obsessive-Compulsive and Related Disorders
15.5 Post-Traumatic Stress Disorder
15.6 Mood Disorders
15.7 Schizophrenia
15.8 Dissociative Disorders
15.9 Developmental Disorders
15.10 Personality Disorders
15.1 What Are Psychological Disorders?
Learning Objectives
By the end of this section, you will be able to:
- Understand the problems inherent in defining the concept of psychological disorder
- Describe what is meant by harmful dysfunction
- Identify the formal criteria that thoughts, feelings, and behaviors must meet to be considered abnormal and, thus, symptomatic of a psychological disorder
A psychological disorder is a condition characterized by abnormal thoughts, feelings, and behaviors. Psychopathology is the study of psychological disorders, including their symptoms, etiology (i.e., their causes), and treatment. The term psychopathology can also refer to the manifestation of a psychological disorder. Although consensus can be difficult, it is extremely important for mental health professionals to agree on what kinds of thoughts, feelings, and behaviors are truly abnormal in the sense that they genuinely indicate the presence of psychopathology. Certain patterns of behavior and inner experience can easily be labeled as abnormal and clearly signify some kind of psychological disturbance. The person who washes his hands 40 times per day and the person who claims to hear the voices of demons exhibit behaviors and inner experiences that most would regard as abnormal: beliefs and behaviors that suggest the existence of a psychological disorder. But, consider the nervousness a young man feels when talking to an attractive person or the loneliness and longing for home a first-year student experiences during her first semester of college—these feelings may not be regularly present, but they fall in the range of normal. So, what kinds of thoughts, feelings, and behaviors represent a true psychological disorder? Psychologists work to distinguish psychological disorders from inner experiences and behaviors that are merely situational, idiosyncratic, or unconventional.
Definition of a Psychological Disorder
Perhaps the simplest approach to conceptualizing psychological disorders is to label behaviors, thoughts, and inner experiences that are atypical, distressful, dysfunctional, and sometimes even dangerous, as signs of a disorder. For example, if you ask a classmate for a date and you are rejected, you probably would feel a little dejected. Such feelings would be normal. If you felt extremely depressed—so much so that you lost interest in activities, had difficulty eating or sleeping, felt utterly worthless, and contemplated suicide—your feelings would be atypical, would deviate from the norm, and could signify the presence of a psychological disorder. Just because something is atypical, however, does not necessarily mean it is disordered.
For example, only about 4% of people in the United States have red hair, so red hair is considered an atypical characteristic (Figure 15.2), but it is not considered disordered, it’s just unusual. And it is less unusual in Scotland, where approximately 13% of the population has red hair (“DNA Project Aims,” 2012). As you will learn, some disorders, although not exactly typical, are far from atypical, and the rates in which they appear in the population are surprisingly high.
If we can agree that merely being atypical is an insufficient criterion for a having a psychological disorder, is it reasonable to consider behavior or inner experiences that differ from widely expected cultural values or expectations as disordered? Using this criterion, a person who walks around a subway platform wearing a heavy winter coat in July while screaming obscenities at strangers may be considered as exhibiting symptoms of a psychological disorder. Their actions and clothes violate socially accepted rules governing appropriate dress and behavior; these characteristics are atypical.
Cultural Expectations
Violating cultural expectations is not, in and of itself, a satisfactory means of identifying the presence of a psychological disorder. Since behavior varies from one culture to another, what may be expected and considered appropriate in one culture may not be viewed as such in other cultures. For example, returning a stranger’s smile is expected in the United States because a pervasive social norm dictates that we reciprocate friendly gestures. A person who refuses to acknowledge such gestures might be considered socially awkward—perhaps even disordered—for violating this expectation. However, such expectations are not universally shared. Cultural expectations in Japan involve showing reserve, restraint, and a concern for maintaining privacy around strangers. Japanese people are generally unresponsive to smiles from strangers (Patterson et al., 2007). Eye contact provides another example. In the United States and Europe, eye contact with others typically signifies honesty and attention. However, most Latin-American, Asian, and African cultures interpret direct eye contact as rude, confrontational, and aggressive (Pazain, 2010). Thus, someone who makes eye contact with you could be considered appropriate and respectful or brazen and offensive, depending on your culture (Figure 15.3).
Hallucinations (seeing or hearing things that are not physically present) in Western societies is a violation of cultural expectations, and a person who reports such inner experiences is readily labeled as psychologically disordered. In other cultures, visions that, for example, pertain to future events may be regarded as normal experiences that are positively valued (Bourguignon, 1970). Finally, it is important to recognize that cultural norms change over time: what might be considered typical in a society at one time may no longer be viewed this way later, similar to how fashion trends from one era may elicit quizzical looks decades later—imagine how a headband, legwarmers, and the big hair of the 1980s would go over on your campus today.
DIG DEEPER: The Myth of Mental Illness
In the 1950s and 1960s, the concept of mental illness was widely criticized. One of the major criticisms focused on the notion that mental illness was a “myth that justifies psychiatric intervention in socially disapproved behavior” (Wakefield, 1992). Thomas Szasz (1960), a noted psychiatrist, was perhaps the biggest proponent of this view. Szasz argued that the notion of mental illness was invented by society (and the mental health establishment) to stigmatize and subjugate people whose behavior violates accepted social and legal norms. Indeed, Szasz suggested that what appear to be symptoms of mental illness are more appropriately characterized as “problems in living” (Szasz, 1960).
In his 1961 book, The Myth of Mental Illness: Foundations of a Theory of Personal Conduct, Szasz expressed his disdain for the concept of mental illness and for the field of psychiatry in general (Oliver, 2006). The basis for Szasz’s attack was his contention that detectable abnormalities in bodily structures and functions (e.g., infections and organ damage or dysfunction) represent the defining features of genuine illness or disease, and because symptoms of purported mental illness are not accompanied by such detectable abnormalities, so-called psychological disorders are not disorders at all. Szasz (1961/2010) proclaimed that “disease or illness can only affect the body; hence, there can be no mental illness” (p. 267).
Today, we recognize the extreme level of psychological suffering experienced by people with psychological disorders: the painful thoughts and feelings they experience, the disordered behavior they demonstrate, and the levels of distress and impairment they exhibit. This makes it very difficult to deny the reality of mental illness.
However controversial Szasz’s views and those of his supporters might have been, they have influenced the mental health community and society in several ways. First, lay people, politicians, and professionals now often refer to mental illness as mental health “problems,” implicitly acknowledging the “problems in living” perspective Szasz described (Buchanan-Barker & Barker, 2009). Also influential was Szasz’s view of homosexuality. Szasz was perhaps the first psychiatrist to openly challenge the idea that homosexuality represented a form of mental illness or disease (Szasz, 1965). By challenging the idea that homosexuality represented a form a mental illness, Szasz helped pave the way for the social and civil rights that gay and lesbian people now have (Barker, 2010). His work also inspired legal changes that protect the rights of people in psychiatric institutions and allow such individuals a greater degree of influence and responsibility over their lives (Buchanan-Barker & Barker, 2009).
Harmful Dysfunction
If none of the criterion discussed so far is adequate by itself to define the presence of a psychological disorder, how can a disorder be conceptualized? Many efforts have been made to identify the specific dimensions of psychological disorders, yet none is entirely satisfactory. No universal definition of psychological disorder exists that can apply to all situations in which a disorder is thought to be present (Zachar & Kendler, 2007). However, one of the more influential conceptualizations was proposed by Wakefield (1992), who defined psychological disorder as a harmful dysfunction. Wakefield argued that natural internal mechanisms—that is, psychological processes honed by evolution, such as cognition, perception, and learning—have important functions, such as enabling us to experience the world the way others do and to engage in rational thought, problem solving, and communication. For example, learning allows us to associate a fear with a potential danger in such a way that the intensity of fear is roughly equal to the degree of actual danger. Dysfunction occurs when an internal mechanism breaks down and can no longer perform its normal function. But, the presence of a dysfunction by itself does not determine a disorder. The dysfunction must be harmful in that it leads to negative consequences for the individual or for others, as judged by the standards of the individual’s culture. The harm may include significant internal anguish (e.g., high levels of anxiety or depression) or problems in day-to-day living (e.g., in one’s social or work life).
To illustrate, Janet has an extreme fear of spiders. Janet’s fear might be considered a dysfunction in that it signals that the internal mechanism of learning is not working correctly (i.e., a faulty process prevents Janet from appropriately associating the magnitude of fear with the actual threat posed by spiders). Janet’s fear of spiders has a significant negative influence on daily life: they avoids all situations in which they suspect spiders to be present (e.g., the basement or a friend’s home), and they quit her job last month because they saw a spider in the restroom at work and is now unemployed. According to the harmful dysfunction model, Janet’s condition would signify a disorder because (a) there is a dysfunction in an internal mechanism, and (b) the dysfunction has resulted in harmful consequences. Similar to how the symptoms of physical illness reflect dysfunctions in biological processes, the symptoms of psychological disorders presumably reflect dysfunctions in mental processes. The internal mechanism component of this model is especially appealing because it implies that disorders may occur through a breakdown of biological functions that govern various psychological processes, thus supporting contemporary neurobiological models of psychological disorders (Fabrega, 2007).
The American Psychiatric Association (APA) Definition
Many of the features of the harmful dysfunction model are incorporated in a formal definition of psychological disorder developed by the American Psychiatric Association (APA). According to the APA (2013), a psychological disorder is a condition that is said to consist of the following:
- There are significant disturbances in thoughts, feelings, and behaviors. A person must experience inner states (e.g., thoughts and/or feelings) and exhibit behaviors that are clearly disturbed—that is, unusual, but in a negative, self-defeating way. Often, such disturbances are troubling to those around the individual who experiences them. For example, an individual who is uncontrollably preoccupied by thoughts of germs spends hours each day bathing, has inner experiences, and displays behaviors that most would consider atypical and negative (disturbed) and that would likely be troubling to family members.
- The disturbances reflect some kind of biological, psychological, or developmental dysfunction. Disturbed patterns of inner experiences and behaviors should reflect some flaw (dysfunction) in the internal biological, psychological, and developmental mechanisms that lead to normal, healthy psychological functioning. For example, the hallucinations observed in schizophrenia could be a sign of brain abnormalities.
- The disturbances lead to significant distress or disability in one’s life. A person’s inner experiences and behaviors are considered to reflect a psychological disorder if they cause the person considerable distress, or greatly impair his ability to function as a normal individual (often referred to as functional impairment, or occupational and social impairment). As an illustration, a person’s fear of social situations might be so distressing that it causes the person to avoid all social situations (e.g., preventing that person from being able to attend class or apply for a job).
- The disturbances do not reflect expected or culturally approved responses to certain events. Disturbances in thoughts, feelings, and behaviors must be socially unacceptable responses to certain events that often happen in life. For example, it is perfectly natural (and expected) that a person would experience great sadness and might wish to be left alone following the death of a close family member. Because such reactions are in some ways culturally expected, the individual would not be assumed to signify a mental disorder.
Some believe that there is no essential criterion or set of criteria that can definitively distinguish all cases of disorder from nondisorder (Lilienfeld & Marino, 1999). In truth, no single approach to defining a psychological disorder is adequate by itself, nor is there universal agreement on where the boundary is between disordered and not disordered. From time to time we all experience anxiety, unwanted thoughts, and moments of sadness; our behavior at other times may not make much sense to ourselves or to others. These inner experiences and behaviors can vary in their intensity, but are only considered disordered when they are highly disturbing to us and/or others, suggest a dysfunction in normal mental functioning, and are associated with significant distress or disability in social or occupational activities.
15.2 Diagnosing and Classifying Psychological Disorders
Learning Objectives
By the end of this section, you will be able to:
- Explain why classification systems are necessary in the study of psychopathology
- Describe the basic features of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)
- Discuss changes in the DSM over time, including criticisms of the current edition
- Identify which disorders are generally the most common
A first step in the study of psychological disorders is carefully and systematically discerning significant signs and symptoms. How do mental health professionals ascertain whether or not a person’s inner states and behaviors truly represent a psychological disorder? Arriving at a proper diagnosis—that is, appropriately identifying and labeling a set of defined symptoms—is absolutely crucial. This process enables professionals to use a common language with others in the field and aids in communication about the disorder with the patient, colleagues and the public. A proper diagnosis is an essential element to guide proper and successful treatment. For these reasons, classification systems that organize psychological disorders systematically are necessary.
The Diagnostic and Statistical Manual of Mental Disorders (DSM)
Although a number of classification systems have been developed over time, the one that is used by most mental health professionals in the United States is the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association (2013). (Note that the American Psychiatric Association differs from the American Psychological Association; both are abbreviated APA.) The first edition of the DSM, published in 1952, classified psychological disorders according to a format developed by the U.S. Army during World War II (Clegg, 2012). In the years since, the DSM has undergone numerous revisions and editions. The most recent edition, published in 2013, is the DSM-5 (APA, 2013). The DSM-5 includes many categories of disorders (e.g., anxiety disorders, depressive disorders, and dissociative disorders). Each disorder is described in detail, including an overview of the disorder (diagnostic features), specific symptoms required for diagnosis (diagnostic criteria), prevalence information (what percent of the population is thought to be afflicted with the disorder), and risk factors associated with the disorder. Figure 15.4 shows lifetime prevalence rates—the percentage of people in a population who develop a disorder in their lifetime—of various psychological disorders among U.S. adults. These data were based on a national sample of 9,282 U.S. residents (National Comorbidity Survey, 2007).
The DSM-5 also provides information about comorbidity; the co-occurrence of two disorders. For example, the DSM-5 mentions that 41% of people with obsessive-compulsive disorder (OCD) also meet the diagnostic criteria for major depressive disorder (Figure 15.5). Drug use is highly comorbid with other mental illnesses; 6 out of 10 people who have a substance use disorder also suffer from another form of mental illness (National Institute on Drug Abuse [NIDA], 2007).
CONNECT THE CONCEPTS: Comorbidity
As you’ve learned in the text, comorbidity refers to situations in which an individual suffers from more than one disorder, and often the symptoms of each can interact in negative ways. Co-occurrence and comorbidity of psychological disorders are quite common, and some of the most pervasive comorbidities involve substance use disorders that co-occur with psychological disorders. Indeed, some estimates suggest that around a quarter of people who suffer from the most severe cases of mental illness exhibit substance use disorder as well. Conversely, around 10 percent of individuals seeking treatment for substance use disorder have serious mental illnesses. Observations such as these have important implications for treatment options that are available. When people with a mental illness are also habitual drug users, their symptoms can be exacerbated and resistant to treatment. Furthermore, it is not always clear whether the symptoms are due to drug use, the mental illness, or a combination of the two. Therefore, it is recommended that behavior is observed in situations in which the individual has ceased using drugs and is no longer experiencing withdrawal from the drug in order to make the most accurate diagnosis (NIDA, 2018).
Obviously, substance use disorders are not the only possible comorbidities. In fact, some of the most common psychological disorders tend to co-occur. For instance, more than half of individuals who have a primary diagnosis of depressive disorder are estimated to exhibit some sort of anxiety disorder. The reverse is also true for those diagnosed with a primary diagnosis of an anxiety disorder. Further, anxiety disorders and major depression have a high rate of comorbidity with several other psychological disorders (Al-Asadi, Klein, & Meyer, 2015).
The DSM has changed considerably in the half-century since it was originally published. The first two editions of the DSM, for example, listed homosexuality as a disorder; however, in 1973, the APA voted to remove it from the manual (Silverstein, 2009). While the DSM-III did not list homosexuality as a disorder, it introduced a new diagnosis, ego-dystonic homosexuality, which emphasized homosexual arousal that the patient viewed as interfering with desired heterosexual relationships and causing distress for the individual. This new diagnosis was considered by many as a compromise to appease those who viewed homosexuality as a mental illness. Other professionals questioned how appropriate it was to have a separate diagnosis that described the content of an individual’s distress. In 1986, the diagnosis was removed from the DSM-III-R (Herek, 2012). Additionally, beginning with the DSM-III in 1980, mental disorders have been described in much greater detail, and the number of diagnosable conditions has grown steadily, as has the size of the manual itself. DSM-I included 106 diagnoses and was 130 total pages, whereas DSM-III included more than 2 times as many diagnoses (265) and was nearly seven times its size (886 total pages) (Mayes & Horowitz, 2005). Although DSM-5 is longer than DSM-IV, the volume includes only 237 disorders, a decrease from the 297 disorders that were listed in DSM-IV. The latest edition, DSM-5, includes revisions in the organization and naming of categories and in the diagnostic criteria for various disorders (Regier, Kuhl, & Kupfer, 2012), while emphasizing careful consideration of the importance of gender and cultural difference in the expression of various symptoms (Fisher, 2010).
Some believe that establishing new diagnoses might overpathologize the human condition by turning common human problems into mental illnesses (The Associated Press, 2013). Indeed, the finding that nearly half of all Americans will meet the criteria for a DSM disorder at some point in their life (Kessler et al., 2005) likely fuels much of this skepticism. The DSM-5 is also criticized on the grounds that its diagnostic criteria have been loosened, thereby threatening to “turn our current diagnostic inflation into diagnostic hyperinflation” (Frances, 2012, para. 22). For example, DSM-IV specified that the symptoms of major depressive disorder must not be attributable to normal bereavement (loss of a loved one). The DSM-5, however, has removed this bereavement exclusion, essentially meaning that grief and sadness after a loved one’s death can constitute major depressive disorder.
The International Classification of Diseases
A second classification system, the International Classification of Diseases (ICD), is also widely recognized. Published by the World Health Organization (WHO), the ICD was developed in Europe shortly after World War II and, like the DSM, has been revised several times. The categories of psychological disorders in both the DSM and ICD are similar, as are the criteria for specific disorders; however, some differences exist. Although the ICD is used for clinical purposes, this tool is also used to examine the general health of populations and to monitor the prevalence of diseases and other health problems internationally (WHO, 2013). The ICD is in its 10th edition (ICD-10); however, efforts are now underway to develop a new edition (ICD-11) that, in conjunction with the changes in DSM-5, will help harmonize the two classification systems as much as possible (APA, 2013).
A study that compared the use of the two classification systems found that worldwide the ICD is more frequently used for clinical diagnosis, whereas the DSM is more valued for research (Mezzich, 2002). Most research findings concerning the etiology and treatment of psychological disorders are based on criteria set forth in the DSM (Oltmanns & Castonguay, 2013). The DSM also includes more explicit disorder criteria, along with an extensive and helpful explanatory text (Regier et al., 2012). The DSM is the classification system of choice among U.S. mental health professionals, and this chapter is based on the DSM paradigm.
The Compassionate View of Psychological Disorders
As these disorders are outlined, please bear two things in mind. First, remember that psychological disorders represent extremes of inner experience and behavior. If, while reading about these disorders, you feel that these descriptions begin to personally characterize you, do not worry—this moment of enlightenment probably means nothing more than you are normal. Each of us experiences episodes of sadness, anxiety, and preoccupation with certain thoughts—times when we do not quite feel ourselves. These episodes should not be considered problematic unless the accompanying thoughts and behaviors become extreme and have a disruptive effect on one’s life. Second, understand that people with psychological disorders are far more than just embodiments of their disorders. We do not use terms such as schizophrenics, depressives, or phobics because they are labels that objectify people who suffer from these conditions, thus promoting biased and disparaging assumptions about them. It is important to remember that a psychological disorder is not what a person is; it is something that a person has—through no fault of his or her own. As is the case with cancer or diabetes, those with psychological disorders suffer debilitating, often painful conditions that are not of their own choosing. These individuals deserve to be viewed and treated with compassion, understanding, and dignity.
Learning Objectives
By the end of this section, you will be able to:
- Discuss supernatural perspectives on the origin of psychological disorders, in their historical context
- Describe modern biological and psychological perspectives on the origin of psychological disorders
- Identify which disorders generally show the highest degree of heritability
- Describe the diathesis-stress model and its importance to the study of psychopathology
Scientists, mental health professionals, and cultural healers may adopt different perspectives in attempting to understand or explain the underlying mechanisms that contribute to the development of a psychological disorder. The specific perspective used in explaining a psychological disorder is extremely important. Each perspective explains psychological disorders, their causes or etiology, and effective treatments from a different viewpoint. Different perspectives provide alternate ways for how to think about the nature of psychopathology.
Supernatural Perspectives of Psychological Disorders
For centuries, psychological disorders were viewed from a supernatural perspective: attributed to a force beyond scientific understanding. Those afflicted were thought to be practitioners of black magic or possessed by spirits (Figure 15.6) (Maher & Maher, 1985). For example, convents throughout Europe in the 16th and 17th centuries reported hundreds of nuns falling into a state of frenzy in which the afflicted foamed at the mouth, screamed and convulsed, sexually propositioned priests, and confessed to having carnal relations with devils or Christ. Although, today, these cases would suggest serious mental illness; at the time, these events were routinely explained as possession by devilish forces (Waller, 2009a). Similarly, grievous fits by young girls are believed to have precipitated the witch panic in New England late in the 17th century (Demos, 1983). Such beliefs in supernatural causes of mental illness are still held in some societies today; for example, beliefs that supernatural forces cause mental illness are common in some cultures in modern-day Nigeria (Aghukwa, 2012).
DIG DEEPER: Dancing Mania
Between the 11th and 17th centuries, a curious epidemic swept across Western Europe. Groups of people would suddenly begin to dance with wild abandon. This compulsion to dance—referred to as dancing mania—sometimes gripped thousands of people at a time (Figure 15.7). Historical accounts indicate that those afflicted would sometimes dance with bruised and bloody feet for days or weeks, screaming of terrible visions and begging priests and monks to save their souls (Waller, 2009b). What caused dancing mania is not known, but several explanations have been proposed, including spider venom and ergot poisoning (“Dancing Mania,” 2011).

Historian John Waller (2009a, 2009b) has provided a comprehensive and convincing explanation of dancing mania that suggests the phenomenon was attributable to a combination of three factors: psychological distress, social contagion, and belief in supernatural forces. Waller argued that various disasters of the time (such as famine, plagues, and floods) produced high levels of psychological distress that could increase the likelihood of succumbing to an involuntary trance state. Waller indicated that anthropological studies and accounts of possession rituals show that people are more likely to enter a trance state if they expect it to happen, and that entranced individuals behave in a ritualistic manner, their thoughts and behavior shaped by the spiritual beliefs of their culture. Thus, during periods of extreme physical and mental distress, all it took were a few people—believing themselves to have been afflicted with a dancing curse—to slip into a spontaneous trance and then act out the part of one who is cursed by dancing for days on end.
Biological Perspectives of Psychological Disorders
The biological perspective views psychological disorders as linked to biological phenomena, such as genetic factors, chemical imbalances, and brain abnormalities; it has gained considerable attention and acceptance in recent decades (Wyatt & Midkiff, 2006). Evidence from many sources indicates that most psychological disorders have a genetic component; in fact, there is little dispute that some disorders are largely due to genetic factors. The graph in Figure 15.8 shows heritability estimates for schizophrenia.
Findings such as these have led many of today’s researchers to search for specific genes and genetic mutations that contribute to mental disorders. Also, sophisticated neural imaging technology in recent decades has revealed how abnormalities in brain structure and function might be directly involved in many disorders, and advances in our understanding of neurotransmitters and hormones have yielded insights into their possible connections. The biological perspective is currently thriving in the study of psychological disorders.
The Diathesis-Stress Model of Psychological Disorders
Despite advances in understanding the biological basis of psychological disorders, the psychosocial perspective is still very important. This perspective emphasizes the importance of learning, stress, faulty and self-defeating thinking patterns, and environmental factors. Perhaps the best way to think about psychological disorders, then, is to view them as originating from a combination of biological and psychological processes. Many develop not from a single cause, but from a delicate fusion between partly biological and partly psychosocial factors.
The diathesis-stress model (Zuckerman, 1999) integrates biological and psychosocial factors to predict the likelihood of a disorder. This diathesis-stress model suggests that people with an underlying predisposition for a disorder (i.e., a diathesis) are more likely than others to develop a disorder when faced with adverse environmental or psychological events (i.e., stress), such as childhood maltreatment, negative life events, trauma, and so on. A diathesis is not always a biological vulnerability to an illness; some diatheses may be psychological (e.g., a tendency to think about life events in a pessimistic, self-defeating way).
The key assumption of the diathesis-stress model is that both factors, diathesis and stress, are necessary in the development of a disorder. Different models explore the relationship between the two factors: the level of stress needed to produce the disorder is inversely proportional to the level of diathesis.
15.3 Anxiety Disorders
Learning Objectives
By the end of this section, you will be able to:
- Distinguish normal anxiety from pathological anxiety
- List and describe the major anxiety disorders, including their main features and prevalence
- Describe basic psychological and biological factors that are suspected to be important in the etiology of anxiety disorder
Everybody experiences anxiety from time to time. Although anxiety is closely related to fear, the two states possess important differences. Fear involves an instantaneous reaction to an imminent threat, whereas anxiety involves apprehension, avoidance, and cautiousness regarding a potential threat, danger, or other negative event (Craske, 1999). While anxiety is unpleasant to most people, it is important to our health, safety, and well-being. Anxiety motivates us to take actions—such as preparing for exams, watching our weight, showing up to work on time—that enable us to avert potential future problems. Anxiety also motivates us to avoid certain things—such as running up debts and engaging in illegal activities—that could lead to future trouble. Most individuals’ level and duration of anxiety approximates the magnitude of the potential threat they face. For example, suppose a student who came to the U.S. as a “Dreamer” (someone whose parents didn’t lawfully immigrate) is concerned about the possibility of being unable to continue in the university program or of losing access to academic financial aid, due to changes and litigation around the Deferred Action for Childhood Arrivals (DACA) program. This person likely would experience anxiety of greater intensity and duration than would a 21-year-old junior who entered college as a birthright citizen. Some people experience anxiety that is excessive, persistent, and greatly out of proportion to the actual threat; if one’s anxiety has a disruptive influence on one’s life, this is a strong indicator that the individual is experiencing an anxiety disorder.
Anxiety disorders are characterized by excessive and persistent fear and anxiety, and by related disturbances in behavior (APA, 2013). Although anxiety is universally experienced, anxiety disorders cause considerable distress. As a group, anxiety disorders are common: approximately 25%–30% of the U.S. population meets the criteria for at least one anxiety disorder during their lifetime (Kessler et al., 2005). Also, these disorders appear to be much more common in women than they are in men; within a 12-month period, around 23% of women and 14% of men will experience at least one anxiety disorder (National Comorbidity Survey, 2007). Anxiety disorders are the most frequently occurring class of mental disorders and are often comorbid with each other and with other mental disorders (Kessler, Ruscio, Shear, & Wittchen, 2009).
Specific Phobia
Phobia is a Greek word that means fear. A person diagnosed with a specific phobia (formerly known as simple phobia) experiences excessive, distressing, and persistent fear or anxiety about a specific object or situation (such as animals, enclosed spaces, elevators, or flying) (APA, 2013). Even though people realize their level of fear and anxiety in relation to the phobic stimulus is irrational, some people with a specific phobia may go to great lengths to avoid the phobic stimulus (the object or situation that triggers the fear and anxiety). Typically, the fear and anxiety a phobic stimulus elicits is disruptive to the person’s life. For example, a man with a phobia of flying might refuse to accept a job that requires frequent air travel, thus negatively affecting his career. Clinicians who have worked with people who have specific phobias have encountered many kinds of phobias, some of which are shown in Table 15.1.
| Specific Phobias | |
|---|---|
| Phobia | Feared Object or Situation |
| Acrophobia | heights |
| Aerophobia | flying |
| Arachnophobia | spiders |
| Claustrophobia | enclosed spaces |
| Cynophobia | dogs |
| Hematophobia | blood |
| Ophidiophobia | snakes |
| Taphophobia | being buried alive |
| Trypanophobia | injections |
| Xenophobia | strangers |
Specific phobias are common; in the United States, around 12.5% of the population will meet the criteria for a specific phobia at some point in their lifetime (Kessler et al., 2005). One type of phobia, agoraphobia, is listed in the DSM-5 as a separate anxiety disorder. Agoraphobia, which literally means “fear of the marketplace,” is characterized by intense fear, anxiety, and avoidance of situations in which it might be difficult to escape or receive help if one experiences symptoms of a panic attack (a state of extreme anxiety that we will discuss shortly). These situations include public transportation, open spaces (parking lots), enclosed spaces (stores), crowds, or being outside the home alone (APA, 2013). About 1.4% of Americans experience agoraphobia during their lifetime (Kessler et al., 2005).
Acquisition of Phobias Through Learning
Many theories suggest that phobias develop through learning. Rachman (1977) proposed that phobias can be acquired through three major learning pathways. The first pathway is through classical conditioning. As you may recall, classical conditioning is a form of learning in which a previously neutral stimulus is paired with an unconditioned stimulus (UCS) that reflexively elicits an unconditioned response (UCR), eliciting the same response through its association with the unconditioned stimulus. The response is called a conditioned response (CR). For example, a child who has been bitten by a dog may come to fear dogs because of a past association with pain. In this case, the dog bite is the UCS and the fear it elicits is the UCR. Because a dog was associated with the bite, any dog may come to serve as a conditioned stimulus, thereby eliciting fear; the fear the child experiences around dogs, then, becomes a CR.
The second pathway of phobia acquisition is through vicarious learning, such as modeling. For example, a child who observes his cousin react fearfully to spiders may later express the same fears, even though spiders have never presented any danger to him. This phenomenon has been observed in both humans and nonhuman primates (Olsson & Phelps, 2007). A study of laboratory-reared monkeys readily acquired a fear of snakes after observing wild-reared monkeys react fearfully to snakes (Mineka & Cook, 1993).
The third pathway is through verbal transmission or information. For example, a child whose parents, siblings, friends, and classmates constantly tell her how disgusting and dangerous snakes are may come to acquire a fear of snakes.
Interestingly, people are more likely to develop phobias of things that do not represent much actual danger to themselves, such as animals and heights, and are less likely to develop phobias toward things that present legitimate danger in contemporary society, such as motorcycles and weapons (Öhman & Mineka, 2001). Why might this be so? One theory suggests that the human brain is evolutionarily predisposed to more readily associate certain objects or situations with fear (Seligman, 1971). This theory argues that throughout our evolutionary history, our ancestors associated certain stimuli (e.g., snakes, spiders, heights, and thunder) with potential danger. As time progressed, the mind has become adapted to more readily develop fears of these things than of others. Experimental evidence has consistently demonstrated that conditioned fears develop more readily to fear-relevant stimuli (images of snakes and spiders) than to fear-irrelevant stimuli (images of flowers and berries) (Öhman & Mineka, 2001). Such prepared learning has also been shown to occur in monkeys. In one study (Cook & Mineka, 1989), monkeys watched videotapes of model monkeys reacting fearfully to either fear-relevant stimuli (toy snakes or a toy crocodile) or fear-irrelevant stimuli (flowers or a toy rabbit). The observer monkeys developed fears of the fear-relevant stimuli but not the fear-irrelevant stimuli.
Social Anxiety Disorder
Social anxiety disorder (formerly called social phobia) is characterized by extreme and persistent fear or anxiety and avoidance of social situations in which the person could potentially be evaluated negatively by others (APA, 2013). As with specific phobias, social anxiety disorder is common in the United States; a little over 12% of all Americans experience social anxiety disorder during their lifetime (Kessler et al., 2005).
The heart of the fear and anxiety in social anxiety disorder is the person’s concern that he may act in a humiliating or embarrassing way, such as appearing foolish, showing symptoms of anxiety (blushing), or doing or saying something that might lead to rejection (such as offending others). The kinds of social situations in which individuals with social anxiety disorder usually have problems include public speaking, having a conversation, meeting strangers, eating in restaurants, and, in some cases, using public restrooms. Although many people become anxious in social situations like public speaking, the fear, anxiety, and avoidance experienced in social anxiety disorder are highly distressing and lead to serious impairments in life. Adults with this disorder are more likely to experience lower educational attainment and lower earnings (Katzelnick et al., 2001), perform more poorly at work and are more likely to be unemployed (Moitra, Beard, Weisberg, & Keller, 2011), and report greater dissatisfaction with their family lives, friends, leisure activities, and income (Stein & Kean, 2000).
When people with social anxiety disorder are unable to avoid situations that provoke anxiety, they typically perform safety behaviors: mental or behavioral acts that reduce anxiety in social situations by reducing the chance of negative social outcomes. Safety behaviors include avoiding eye contact, rehearsing sentences before speaking, talking only briefly, and not talking about oneself (Alden & Bieling, 1998). Other examples of safety behaviors include the following (Marker, 2013):
- assuming roles in social situations that minimize interaction with others (e.g., taking pictures, setting up equipment, or helping prepare food)
- asking people many questions to keep the focus off of oneself
- selecting a position to avoid scrutiny or contact with others (sitting in the back of the room)
- wearing bland, neutral clothes to avoid drawing attention to oneself
- avoiding substances or activities that might cause anxiety symptoms (such as caffeine, warm clothing, and physical exercise)
Although these behaviors are intended to prevent the person with social anxiety disorder from doing something awkward that might draw criticism, these actions usually exacerbate the problem because they do not allow the individual to disconfirm his negative beliefs, often eliciting rejection and other negative reactions from others (Alden & Bieling, 1998).
People with social anxiety disorder may resort to self-medication, such as drinking alcohol, as a means to avert the anxiety symptoms they experience in social situations (Battista & Kocovski, 2010). The use of alcohol when faced with such situations may become negatively reinforcing: encouraging individuals with social anxiety disorder to turn to the substance whenever they experience anxiety symptoms. The tendency to use alcohol as a coping mechanism for social anxiety, however, can come with a hefty price tag: a number of large scale studies have reported a high rate of comorbidity between social anxiety disorder and alcohol use disorder (Morris, Stewart, & Ham, 2005).
As with specific phobias, it is highly probable that the fears inherent to social anxiety disorder can develop through conditioning experiences. For example, a child who is subjected to early unpleasant social experiences (e.g., bullying at school) may develop negative social images of herself that become activated later in anxiety-provoking situations (Hackmann, Clark, & McManus, 2000). Indeed, one study reported that 92% of a sample of adults with social anxiety disorder reported a history of severe teasing in childhood, compared to only 35% of a sample of adults with panic disorder (McCabe, Antony, Summerfeldt, Liss, & Swinson, 2003).
One of the most well-established risk factors for developing social anxiety disorder is behavioral inhibition (Clauss & Blackford, 2012). Behavioral inhibition is thought to be an inherited trait, and it is characterized by a consistent tendency to show fear and restraint when presented with unfamiliar people or situations (Kagan, Reznick, & Snidman, 1988). Behavioral inhibition is displayed very early in life; behaviorally inhibited toddlers and children respond with great caution and restraint in unfamiliar situations, and they are often timid, fearful, and shy around unfamiliar people (Fox, Henderson, Marshall, Nichols, & Ghera, 2005). A recent statistical review of studies demonstrated that behavioral inhibition was associated with more than a sevenfold increase in the risk of development of social anxiety disorder, demonstrating that behavioral inhibition is a major risk factor for the disorder (Clauss & Blackford, 2012).
Panic Disorder
Imagine that you are at the mall one day with your friends and—suddenly and inexplicably—you begin sweating and trembling, your heart starts pounding, you have trouble breathing, and you start to feel dizzy and nauseous. This episode lasts for 10 minutes and is terrifying because you start to think that you are going to die. When you visit your doctor the following morning and describe what happened, she tells you that you have experienced a panic attack (Figure 15.9). If you experience another one of these episodes two weeks later and worry for a month or more that similar episodes will occur in the future, it is likely that you have developed panic disorder.
People with panic disorder experience recurrent (more than one) and unexpected panic attacks, along with at least one month of persistent concern about additional panic attacks, worry over the consequences of the attacks, or self-defeating changes in behavior related to the attacks (e.g., avoidance of exercise or unfamiliar situations) (APA, 2013). As is the case with other anxiety disorders, the panic attacks cannot result from the physiological effects of drugs and other substances, a medical condition, or another mental disorder. A panic attack is defined as a period of extreme fear or discomfort that develops abruptly and reaches a peak within 10 minutes. Its symptoms include accelerated heart rate, sweating, trembling, choking sensations, hot flashes or chills, dizziness or lightheadedness, fears of losing control or going crazy, and fears of dying (APA, 2013). Sometimes panic attacks are expected, occurring in response to specific environmental triggers (such as being in a tunnel); other times, these episodes are unexpected and emerge randomly (such as when relaxing). According to the DSM-5, the person must experience unexpected panic attacks to qualify for a diagnosis of panic disorder.
Experiencing a panic attack is often terrifying. Rather than recognizing the symptoms of a panic attack merely as signs of intense anxiety, individuals with panic disorder often misinterpret them as a sign that something is intensely wrong internally (thinking, for example, that the pounding heart represents an impending heart attack). Panic attacks can occasionally precipitate trips to the emergency room because several symptoms of panic attacks are, in fact, similar to those associated with heart problems (e.g., palpitations, racing pulse, and a pounding sensation in the chest) (Root, 2000). Unsurprisingly, those with panic disorder fear future attacks and may become preoccupied with modifying their behavior in an effort to avoid future panic attacks. For this reason, panic disorder is often characterized as fear of fear (Goldstein & Chambless, 1978).
Panic attacks themselves are not mental disorders. Indeed, around 23% of Americans experience isolated panic attacks in their lives without meeting the criteria for panic disorder (Kessler et al., 2006), indicating that panic attacks are fairly common. Panic disorder is, of course, much less common, afflicting 4.7% of Americans during their lifetime (Kessler et al., 2005). Many people with panic disorder develop agoraphobia, which is marked by fear and avoidance of situations in which escape might be difficult or help might not be available if one were to develop symptoms of a panic attack. People with panic disorder often experience a comorbid disorder, such as other anxiety disorders or major depressive disorder (APA, 2013).
Researchers are not entirely sure what causes panic disorder. Children are at a higher risk of developing panic disorder if their parents have the disorder (Biederman et al., 2001), and family and twins studies indicate that the heritability of panic disorder is around 43% (Hettema, Neale, & Kendler, 2001). The exact genes and gene functions involved in this disorder, however, are not well-understood (APA, 2013). Neurobiological theories of panic disorder suggest that a region of the brain called the locus coeruleus may play a role in this disorder. Located in the brainstem, the locus coeruleus is the brain’s major source of norepinephrine, a neurotransmitter that triggers the body’s fight-or-flight response. Activation of the locus coeruleus is associated with anxiety and fear, and research with nonhuman primates has shown that stimulating the locus coeruleus either electrically or through drugs produces panic-like symptoms (Charney et al., 1990). Such findings have led to the theory that panic disorder may be caused by abnormal norepinephrine activity in the locus coeruleus (Bremner, Krystal, Southwick, & Charney, 1996).
Conditioning theories of panic disorder propose that panic attacks are classical conditioning responses to subtle bodily sensations resembling those normally occurring when one is anxious or frightened (Bouton, Mineka, & Barlow, 2001). For example, consider a child who has asthma. An acute asthma attack produces sensations, such as shortness of breath, coughing, and chest tightness, that typically elicit fear and anxiety. Later, when the child experiences subtle symptoms that resemble the frightening symptoms of earlier asthma attacks (such as shortness of breath after climbing stairs), he may become anxious, fearful, and then experience a panic attack. In this situation, the subtle symptoms would represent a conditioned stimulus, and the panic attack would be a conditioned response. The finding that panic disorder is nearly three times as frequent among people with asthma as it is among people without asthma (Weiser, 2007) supports the possibility that panic disorder has the potential to develop through classical conditioning.
Cognitive factors may play an integral part in panic disorder. Generally, cognitive theories (Clark, 1996) argue that those with panic disorder are prone to interpret ordinary bodily sensations catastrophically, and these fearful interpretations set the stage for panic attacks. For example, a person might detect bodily changes that are routinely triggered by innocuous events such getting up from a seated position (dizziness), exercising (increased heart rate, shortness of breath), or drinking a large cup of coffee (increased heart rate, trembling). The individual interprets these subtle bodily changes catastrophically (“Maybe I’m having a heart attack!”). Such interpretations create fear and anxiety, which trigger additional physical symptoms; subsequently, the person experiences a panic attack. Support of this contention rests with findings that people with more severe catastrophic thoughts about sensations have more frequent and severe panic attacks, and among those with panic disorder, reducing catastrophic cognitions about their sensations is as effective as medication in reducing panic attacks (Good & Hinton, 2009).
Generalized Anxiety Disorder
Alex was always worried about many things. He worried that his children would drown when they played at the beach. Each time he left the house, he worried that an electrical short circuit would start a fire in his home. He worried that his husband would lose his job at the prestigious law firm. He worried that his daughter’s minor staph infection could turn into a massive life-threatening condition. These and other worries constantly weighed heavily on Alex’s mind, so much so that they made it difficult for him to make decisions and often left him feeling tense, irritable, and worn out. One night, Alex’s husband was to drive their son home from a soccer game. However, his husband stayed after the game and talked with some of the other parents, resulting in her arriving home 45 minutes late. Alex had tried to call his cell phone three or four times, but he could not get through because the soccer field did not have a signal. Extremely worried, Alex eventually called the police, convinced that his husband and son had not arrived home because they had been in a terrible car accident.
Alex suffers from generalized anxiety disorder: a relatively continuous state of excessive, uncontrollable, and pointless worry and apprehension. People with generalized anxiety disorder often worry about routine, everyday things, even though their concerns are unjustified (Figure 15.10). For example, an individual may worry about her health and finances, the health of family members, the safety of her children, or minor matters (e.g., being late for an appointment) without having any legitimate reason for doing so (APA, 2013). A diagnosis of generalized anxiety disorder requires that the diffuse worrying and apprehension characteristic of this disorder—what Sigmund Freud referred to as free-floating anxiety—is not part of another disorder, occurs more days than not for at least six months, and is accompanied by any three of the following symptoms: restlessness, difficulty concentrating, being easily fatigued, muscle tension, irritability, and sleep difficulties.
About 5.7% of the U.S. population will develop symptoms of generalized anxiety disorder during their lifetime (Kessler et al., 2005), and females are 2 times as likely as males to experience the disorder (APA, 2013). Generalized anxiety disorder is highly comorbid with mood disorders and other anxiety disorders (Noyes, 2001), and it tends to be chronic. Also, generalized anxiety disorder appears to increase the risk for heart attacks and strokes, especially in people with preexisting heart conditions (Martens et al., 2010).
Although there have been few investigations aimed at determining the heritability of generalized anxiety disorder, a summary of available family and twin studies suggests that genetic factors play a modest role in the disorder (Hettema et al., 2001). Cognitive theories of generalized anxiety disorder suggest that worry represents a mental strategy to avoid more powerful negative emotions (Aikins & Craske, 2001), perhaps stemming from earlier unpleasant or traumatic experiences. Indeed, one longitudinal study found that childhood maltreatment was strongly related to the development of this disorder during adulthood (Moffitt et al., 2007); worrying might distract people from remembering painful childhood experiences.
15.4 Obsessive-Compulsive and Related Disorders
Learning Objectives
By the end of this section, you will be able to:
- Describe the main features and prevalence of obsessive-compulsive disorder, body dysmorphic disorder, and hoarding disorder
- Understand some of the factors in the development of obsessive-compulsive disorder
Obsessive-compulsive and related disorders are a group of overlapping disorders that generally involve intrusive, unpleasant thoughts and repetitive behaviors. Many of us experience unwanted thoughts from time to time (e.g., craving double cheeseburgers when dieting), and many of us engage in repetitive behaviors on occasion (e.g., pacing when nervous). However, obsessive-compulsive and related disorders elevate the unwanted thoughts and repetitive behaviors to a status so intense that these cognitions and activities disrupt daily life. Included in this category are obsessive-compulsive disorder (OCD), body dysmorphic disorder, and hoarding disorder.
Obsessive-Compulsive Disorder
People with obsessive-compulsive disorder (OCD) experience thoughts and urges that are intrusive and unwanted (obsessions) and/or the need to engage in repetitive behaviors or mental acts (compulsions). A person with this disorder might, for example, spend hours each day washing his hands or constantly checking and rechecking to make sure that a stove, faucet, or light has been turned off.
Obsessions are more than just unwanted thoughts that seem to randomly jump into our head from time to time, such as recalling an insensitive remark a coworker made recently, and they are more significant than day-to-day worries we might have, such as justifiable concerns about being laid off from a job. Rather, obsessions are characterized as persistent, unintentional, and unwanted thoughts and urges that are highly intrusive, unpleasant, and distressing (APA, 2013). Common obsessions include concerns about germs and contamination, doubts (“Did I turn the water off?”), order and symmetry (“I need all the spoons in the tray to be arranged a certain way”), and urges that are aggressive or lustful. Usually, the person knows that such thoughts and urges are irrational and thus tries to suppress or ignore them, but has an extremely difficult time doing so. These obsessive symptoms sometimes overlap, such that someone might have both contamination and aggressive obsessions (Abramowitz & Siqueland, 2013).
Compulsions are repetitive and ritualistic acts that are typically carried out primarily as a means to minimize the distress that obsessions trigger or to reduce the likelihood of a feared event (APA, 2013). Compulsions often include such behaviors as repeated and extensive hand washing, cleaning, checking (e.g., that a door is locked), and ordering (e.g., lining up all the pencils in a particular way), and they also include such mental acts as counting, praying, or reciting something to oneself (Figure 15.11). Compulsions characteristic of OCD are not performed out of pleasure, nor are they connected in a realistic way to the source of the distress or feared event. Approximately 2.3% of the U.S. population will experience OCD in their lifetime (Ruscio, Stein, Chiu, & Kessler, 2010) and, if left untreated, OCD tends to be a chronic condition creating lifelong interpersonal and psychological problems (Norberg, Calamari, Cohen, & Riemann, 2008).
Body Dysmorphic Disorder
An individual with body dysmorphic disorder is preoccupied with a perceived flaw in physical appearance that is either nonexistent or barely noticeable to other people (APA, 2013). These perceived physical defects cause people to think they are unattractive, ugly, hideous, or deformed. These preoccupations can focus on any bodily area, but they typically involve the skin, face, or hair. The preoccupation with imagined physical flaws drives the person to engage in repetitive and ritualistic behavioral and mental acts, such as constantly looking in the mirror, trying to hide the offending body part, comparisons with others, and, in some extreme cases, cosmetic surgery (Phillips, 2005). An estimated 2.4% of the adults in the United States meet the criteria for body dysmorphic disorder, with slightly higher rates in women than in men (APA, 2013).
Hoarding Disorder
Although hoarding was traditionally considered to be a symptom of OCD, considerable evidence suggests that hoarding represents an entirely different disorder (Mataix-Cols et al., 2010). People with hoarding disorder cannot bear to part with personal possessions, regardless of how valueless or useless these possessions are. As a result, these individuals accumulate excessive amounts of usually worthless items that clutter their living areas (Figure 15.12). Often, the quantity of cluttered items is so excessive that the person is unable use his kitchen, or sleep in his bed. People who suffer from this disorder have great difficulty parting with items because they believe the items might be of some later use, or because they form a sentimental attachment to the items (APA, 2013). Importantly, a diagnosis of hoarding disorder is made only if the hoarding is not caused by another medical condition and if the hoarding is not a symptom of another disorder (e.g., schizophrenia) (APA, 2013).
Causes of OCD
The results of family and twin studies suggest that OCD has a moderate genetic component. The disorder is five times more frequent in the first-degree relatives of people with OCD than in people without the disorder (Nestadt et al., 2000). Additionally, the concordance rate of OCD among identical twins is around 57%; however, the concordance rate for fraternal twins is 22% (Bolton, Rijsdijk, O’Connor, Perrin, & Eley, 2007). Studies have implicated about two dozen potential genes that may be involved in OCD; these genes regulate the function of three neurotransmitters: serotonin, dopamine, and glutamate (Pauls, 2010). Many of these studies included small sample sizes and have yet to be replicated. Thus, additional research needs to be done in this area.
A brain region that is believed to play a critical role in OCD is the orbitofrontal cortex (Kopell & Greenberg, 2008), an area of the frontal lobe involved in learning and decision-making (Rushworth, Noonan, Boorman, Walton, & Behrens, 2011) (Figure 15.13). In people with OCD, the orbitofrontal cortex becomes especially hyperactive when they are provoked with tasks in which, for example, they are asked to look at a photo of a toilet or of pictures hanging crookedly on a wall (Simon, Kaufmann, Müsch, Kischkel, & Kathmann, 2010). The orbitofrontal cortex is part of a series of brain regions that, collectively, is called the OCD circuit; this circuit consists of several interconnected regions that influence the perceived emotional value of stimuli and the selection of both behavioral and cognitive responses (Graybiel & Rauch, 2000). As with the orbitofrontal cortex, other regions of the OCD circuit show heightened activity during symptom provocation (Rotge et al., 2008), which suggests that abnormalities in these regions may produce the symptoms of OCD (Saxena, Bota, & Brody, 2001). Consistent with this explanation, people with OCD show a substantially higher degree of connectivity of the orbitofrontal cortex and other regions of the OCD circuit than do those without OCD (Beucke et al., 2013).
The findings discussed above were based on imaging studies, and they highlight the potential importance of brain dysfunction in OCD. However, one important limitation of these findings is the inability to explain differences in obsessions and compulsions. Another limitation is that the correlational relationship between neurological abnormalities and OCD symptoms cannot imply causation (Abramowitz & Siqueland, 2013).
CONNECT THE CONCEPTS: Conditioning and OCD
The symptoms of OCD have been theorized to be learned responses, acquired and sustained as the result of a combination of two forms of learning: classical conditioning and operant conditioning (Mowrer, 1960; Steinmetz, Tracy, & Green, 2001). Specifically, the acquisition of OCD may occur first as the result of classical conditioning, whereby a neutral stimulus becomes associated with an unconditioned stimulus that provokes anxiety or distress. When an individual has acquired this association, subsequent encounters with the neutral stimulus trigger anxiety, including obsessive thoughts; the anxiety and obsessive thoughts (which are now a conditioned response) may persist until she identifies some strategy to relieve it. Relief may take the form of a ritualistic behavior or mental activity that, when enacted repeatedly, reduces the anxiety. Such efforts to relieve anxiety constitute an example of negative reinforcement (a form of operant conditioning). Recall from the chapter on learning that negative reinforcement involves the strengthening of behavior through its ability to remove something unpleasant or aversive. Hence, compulsive acts observed in OCD may be sustained because they are negatively reinforcing, in the sense that they reduce anxiety triggered by a conditioned stimulus.
Suppose an individual with OCD experiences obsessive thoughts about germs, contamination, and disease whenever she encounters a doorknob. What might have constituted a viable unconditioned stimulus? Also, what would constitute the conditioned stimulus, unconditioned response, and conditioned response? What kinds of compulsive behaviors might we expect, and how do they reinforce themselves? What is decreased? Additionally, and from the standpoint of learning theory, how might the symptoms of OCD be treated successfully?
Learning Objectives
By the end of this section, you will be able to:
- Describe the nature and symptoms of posttraumatic stress disorder
- Identify the risk factors associated with this disorder
- Understand the role of learning and cognitive factors in its development
Extremely stressful or traumatic events, such as combat, natural disasters, and terrorist attacks, place the people who experience them at an increased risk for developing psychological disorders such as posttraumatic stress disorder (PTSD). Throughout much of the 20th century, this disorder was called shell shock and combat neurosis because its symptoms were observed in soldiers who had engaged in wartime combat. By the late 1970s it had become clear that women who had experienced sexual traumas (e.g., rape, domestic battery, and incest) often experienced the same set of symptoms as did soldiers (Herman, 1997). The term posttraumatic stress disorder was developed given that these symptoms could happen to anyone who experienced psychological trauma.
A Broader Definition of PTSD
PTSD was listed among the anxiety disorders in previous DSM editions. In DSM-5, it is now listed among a group called Trauma-and-Stressor-Related Disorders. For a person to be diagnosed with PTSD, she must be exposed to, witness, or experience the details of a traumatic experience (e.g., a first responder), one that involves “actual or threatened death, serious injury, or sexual violence” (APA, 2013, p. 271). These experiences can include such events as combat, threatened or actual physical attack, sexual assault, natural disasters, terrorist attacks, and automobile accidents. This criterion makes PTSD the only disorder listed in the DSM in which a cause (extreme trauma) is explicitly specified.
Symptoms of PTSD include intrusive and distressing memories of the event, flashbacks (states that can last from a few seconds to several days, during which the individual relives the event and behaves as if the event were occurring at that moment [APA, 2013]), avoidance of stimuli connected to the event, persistently negative emotional states (e.g., fear, anger, guilt, and shame), feelings of detachment from others, irritability, proneness toward outbursts, and an exaggerated startle response (jumpiness). For PTSD to be diagnosed, these symptoms must occur for at least one month.
Roughly 7% of adults in the United States, including 9.7% of women and 3.6% of men, experience PTSD in their lifetime (National Comorbidity Survey, 2007), with higher rates among people exposed to mass trauma and people whose jobs involve duty-related trauma exposure (e.g., police officers, firefighters, and emergency medical personnel) (APA, 2013). Nearly 21% of residents of areas affected by Hurricane Katrina suffered from PTSD one year following the hurricane (Kessler et al., 2008), and 12.6% of Manhattan residents were observed as having PTSD 2–3 years after the 9/11 terrorist attacks (DiGrande et al., 2008).
Risk Factors For PTSD
Of course, not everyone who experiences a traumatic event will go on to develop PTSD; several factors strongly predict the development of PTSD: trauma experience, greater trauma severity, lack of immediate social support, and more subsequent life stress (Brewin, Andrews, & Valentine, 2000). Traumatic events that involve harm by others (e.g., combat, rape, and sexual molestation) carry greater risk than do other traumas (e.g., natural disasters) (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Women are more likely to have been traumatized because of sexual trauma, childhood neglect, and childhood physical abuse. Men are more likely to have been traumatized by natural disaster, life-threatening accident, and physical violence, either witnessed or directed at them. Adolescent boys are more likely to experience accident, physical assault, and witness death/injury; adolescent girls are more likely to experience rape/sexual assault, intimate partner violence, or unexpected death or injury of a loved one. Assaultive violence and witnessing trauma to others is more prevalent among non-whites when compared to whites. African American males are more likely to be exposed to and victims of violence than males of other races (Kilpatrick, Badour, & Resnick, 2017). A 2012 study found that 27% of corrections officers reported experiencing symptoms of PTSD in the past 30 days. Rates were higher for males (31%) than females (22%) (Spinaris, Denhof, & Kellaway, 2012). A study conducted by Jaegers et al (2019) found that 53.4% of jail correctional officers screened positively for PTSD. PTSD is more prevalent in prison populations than in the general public, with prevalence estimates of 6% in male prisoners and 21% in female prisoners (Facer-Irwin et al, 2019). Factors that increase the risk of PTSD include female gender, low socioeconomic status, low intelligence, personal history of mental disorders, history of childhood adversity (abuse or other trauma during childhood), and family history of mental disorders (Brewin et al., 2000). Personality characteristics such as neuroticism and somatization (the tendency to experience physical symptoms when one encounters stress) have been shown to elevate the risk of PTSD (Bramsen, Dirkzwager, & van der Ploeg, 2000). People who experience childhood adversity and/or traumatic experiences during adulthood are at significantly higher risk of developing PTSD if they possess one or two short versions of a gene that regulates the neurotransmitter serotonin (Xie et al., 2009). This suggests a possible diathesis-stress interpretation of PTSD: its development is influenced by the interaction of psychosocial and biological factors.
Support For Sufferers of PTSD
Research has shown that social support following a traumatic event can reduce the likelihood of PTSD (Ozer, Best, Lipsey, & Weiss, 2003). Social support is often defined as the comfort, advice, and assistance received from relatives, friends, and neighbors. Social support can help individuals cope during difficult times by allowing them to discuss feelings and experiences and providing a sense of being loved and appreciated. A 14-year study of 1,377 American Legionnaires who had served in the Vietnam War found that those who perceived less social support when they came home were more likely to develop PTSD than were those who perceived greater support (Figure 15.14). In addition, those who became involved in the community were less likely to develop PTSD, and they were more likely to experience a remission of PTSD than were those who were less involved (Koenen, Stellman, Stellman, & Sommer, 2003).
Learning and the Development of PTSD
PTSD learning models suggest that some symptoms are developed and maintained through classical conditioning. The traumatic event may act as an unconditioned stimulus that elicits an unconditioned response characterized by extreme fear and anxiety. Cognitive, emotional, physiological, and environmental cues accompanying or related to the event are conditioned stimuli. These traumatic reminders evoke conditioned responses (extreme fear and anxiety) similar to those caused by the event itself (Nader, 2001). A person who was in the vicinity of the Twin Towers during the 9/11 terrorist attacks and who developed PTSD may display excessive hypervigilance and distress when planes fly overhead; this behavior constitutes a conditioned response to the traumatic reminder (conditioned stimulus of the sight and sound of an airplane). Differences in how conditionable individuals are help to explain differences in the development and maintenance of PTSD symptoms (Pittman, 1988). Conditioning studies demonstrate facilitated acquisition of conditioned responses and delayed extinction of conditioned responses in people with PTSD (Orr et al., 2000).
Cognitive factors are important in the development and maintenance of PTSD. One model suggests that two key processes are crucial: disturbances in memory for the event, and negative appraisals of the trauma and its aftermath (Ehlers & Clark, 2000). According to this theory, some people who experience traumas do not form coherent memories of the trauma; memories of the traumatic event are poorly encoded and, thus, are fragmented, disorganized, and lacking in detail. Therefore, these individuals are unable remember the event in a way that gives it meaning and context. A rape victim who cannot coherently remember the event may remember only bits and pieces (e.g., the attacker repeatedly telling her she is stupid); because she was unable to develop a fully integrated memory, the fragmentary memory tends to stand out. Although unable to retrieve a complete memory of the event, she may be haunted by intrusive fragments involuntarily triggered by stimuli associated with the event (e.g., memories of the attacker’s comments when encountering a person who resembles the attacker). This interpretation fits previously discussed material concerning PTSD and conditioning. The model also proposes that negative appraisals of the event (“I deserved to be raped because I’m stupid”) may lead to dysfunctional behavioral strategies (e.g., avoiding social activities where men are likely to be present) that maintain PTSD symptoms by preventing both a change in the nature of the memory and a change in the problematic appraisals.
15.6 Mood Disorders
Learning Objectives
By the end of this section, you will be able to:
- Distinguish normal states of sadness and euphoria from states of depression and mania
- Describe the symptoms of major depressive disorder and bipolar disorder
- Understand the differences between major depressive disorder and persistent depressive disorder, and identify two subtypes of depression
- Define the criteria for a manic episode
- Understand genetic, biological, and psychological explanations of major depressive disorder
- Discuss the relationship between mood disorders and suicidal ideation, as well as factors associated with suicide
Blake cries all day and feeling that he is worthless and his life is hopeless, he cannot get out of bed. Crystal stays up all night, talks very rapidly, and went on a shopping spree in which she spent $3,000 on furniture, although she cannot afford it. Maria recently had a baby, and she feels overwhelmed, teary, anxious, and panicked, and believes she is a terrible mother—practically every day since the baby was born. All these individuals demonstrate symptoms of a potential mood disorder.
Mood disorders (Figure 15.15) are characterized by severe disturbances in mood and emotions—most often depression, but also mania and elation (Rothschild, 1999). All of us experience fluctuations in our moods and emotional states, and often these fluctuations are caused by events in our lives. We become elated if our favorite team wins the World Series and dejected if a romantic relationship ends or if we lose our job. At times, we feel fantastic or miserable for no clear reason. People with mood disorders also experience mood fluctuations, but their fluctuations are extreme, distort their outlook on life, and impair their ability to function.
The DSM-5 lists two general categories of mood disorders. Depressive disorders are a group of disorders in which depression is the main feature. Depression is a vague term that, in everyday language, refers to an intense and persistent sadness. Depression is a heterogeneous mood state—it consists of a broad spectrum of symptoms that range in severity. Depressed people feel sad, discouraged, and hopeless. These individuals lose interest in activities once enjoyed, often experience a decrease in drives such as hunger and sex, and frequently doubt personal worth. Depressive disorders vary by degree, but this chapter highlights the most well-known: major depressive disorder (sometimes called unipolar depression).
Bipolar and related disorders are a group of disorders in which mania is the defining feature. Mania is a state of extreme elation and agitation. When people experience mania, they may become extremely talkative, behave recklessly, or attempt to take on many tasks simultaneously. The most recognized of these disorders is bipolar disorder.
Major Depressive Disorder
According to the DSM-5, the defining symptoms of major depressive disorder include “depressed mood most of the day, nearly every day” (feeling sad, empty, hopeless, or appearing tearful to others), and loss of interest and pleasure in usual activities (APA, 2013). In addition to feeling overwhelmingly sad most of each day, people with depression will no longer show interest or enjoyment in activities that previously were gratifying, such as hobbies, sports, sex, social events, time spent with family, and so on. Friends and family members may notice that the person has completely abandoned previously enjoyed hobbies; for example, an avid tennis player who develops major depressive disorder no longer plays tennis (Rothschild, 1999).
To receive a diagnosis of major depressive disorder, one must experience a total of five symptoms for at least a two-week period; these symptoms must cause significant distress or impair normal functioning, and they must not be caused by substances or a medical condition. At least one of the two symptoms mentioned above must be present, plus any combination of the following symptoms (APA, 2013):
- significant weight loss (when not dieting) or weight gain and/or significant decrease or increase in appetite;
- difficulty falling asleep or sleeping too much;
- psychomotor agitation (the person is noticeably fidgety and jittery, demonstrated by behaviors like the inability to sit, pacing, hand-wringing, pulling or rubbing of the skin, clothing, or other objects) or psychomotor retardation (the person talks and moves slowly, for example, talking softly, very little, or in a monotone);
- fatigue or loss of energy;
- feelings of worthlessness or guilt;
- difficulty concentrating and indecisiveness; and
- suicidal ideation: thoughts of death (not just fear of dying), thinking about or planning suicide, or making an actual suicide attempt.
Major depressive disorder is considered episodic: its symptoms are typically present at their full magnitude for a certain period of time and then gradually abate. Approximately 50%–60% of people who experience an episode of major depressive disorder will have a second episode at some point in the future; those who have had two episodes have a 70% chance of having a third episode, and those who have had three episodes have a 90% chance of having a fourth episode (Rothschild, 1999). Although the episodes can last for months, a majority a people diagnosed with this condition (around 70%) recover within a year. However, a substantial number do not recover; around 12% show serious signs of impairment associated with major depressive disorder after 5 years (Boland & Keller, 2009). In the long-term, many who do recover will still show minor symptoms that fluctuate in their severity (Judd, 2012).
Results of Major Depressive Disorder
Major depressive disorder is a serious and incapacitating condition that can have a devastating effect on the quality of one’s life. The person suffering from this disorder lives a profoundly miserable existence that often results in unavailability for work or education, abandonment of promising careers, and lost wages; occasionally, the condition requires hospitalization. The majority of those with major depressive disorder report having faced some kind of discrimination, and many report that having received such treatment has stopped them from initiating close relationships, applying for jobs for which they are qualified, and applying for education or training (Lasalvia et al., 2013). Major depressive disorder also takes a toll on health. Depression is a risk factor for the development of heart disease in healthy patients, as well as adverse cardiovascular outcomes in patients with preexisting heart disease (Whooley, 2006).
Risk Factors for Major Depressive Disorder
Major depressive disorder is often referred to as the common cold of psychiatric disorders. Around 6.6% of the U.S. population experiences major depressive disorder each year; 16.9% will experience the disorder during their lifetime (Kessler & Wang, 2009). It is more common among women than among men, affecting approximately 20% of women and 13% of men at some point in their life (National Comorbidity Survey, 2007). The greater risk among women is not accounted for by a tendency to report symptoms or to seek help more readily, suggesting that gender differences in the rates of major depressive disorder may reflect biological and gender-related environmental experiences (Kessler, 2003).
Lifetime rates of major depressive disorder tend to be highest in North and South America, Europe, and Australia; they are considerably lower in Asian countries (Hasin, Fenton, & Weissman, 2011). The rates of major depressive disorder are higher among younger age cohorts than among older cohorts, perhaps because people in younger age cohorts are more willing to admit depression (Kessler & Wang, 2009).
A number of risk factors are associated with major depressive disorder: unemployment (including homemakers); earning less than $20,000 per year; living in urban areas; or being separated, divorced, or widowed (Hasin et al., 2011). Comorbid disorders include anxiety disorders and substance abuse disorders (Kessler & Wang, 2009).
Subtypes of Depression
The DSM-5 lists several different subtypes of depression. These subtypes—what the DSM-5 refer to as specifiers—are not specific disorders; rather, they are labels used to indicate specific patterns of symptoms or to specify certain periods of time in which the symptoms may be present. One subtype, seasonal pattern, applies to situations in which a person experiences the symptoms of major depressive disorder only during a particular time of year (e.g., fall or winter). In everyday language, people often refer to this subtype as the winter blues.
Another subtype, peripartum onset (commonly referred to as postpartum depression), applies to women who experience major depression during pregnancy or in the four weeks following the birth of their child (APA, 2013). These women often feel very anxious and may even have panic attacks. They may feel guilty, agitated, and be weepy. They may not want to hold or care for their newborn, even in cases in which the pregnancy was desired and intended. In extreme cases, the mother may have feelings of wanting to harm her child or herself. In a horrific illustration, a woman named Andrea Yates, who suffered from extreme peripartum-onset depression (as well as other mental illnesses), drowned her five children in a bathtub (Roche, 2002). Most women with peripartum-onset depression do not physically harm their children, but most do have difficulty being adequate caregivers (Fields, 2010). A surprisingly high number of women experience symptoms of peripartum-onset depression. A study of 10,000 women who had recently given birth found that 14% screened positive for peripartum-onset depression, and that nearly 20% reported having thoughts of wanting to harm themselves (Wisner et al., 2013).
People with persistent depressive disorder (previously known as dysthymia) experience depressed moods most of the day nearly every day for at least two years, as well as at least two of the other symptoms of major depressive disorder. People with persistent depressive disorder are chronically sad and melancholy, but do not meet all the criteria for major depression. However, episodes of full-blown major depressive disorder can occur during persistent depressive disorder (APA, 2013).
Bipolar Disorder
A person with bipolar disorder (commonly known as manic depression) often experiences mood states that vacillate between depression and mania; that is, the person’s mood is said to alternate from one emotional extreme to the other (in contrast to unipolar, which indicates a persistently sad mood).
To be diagnosed with bipolar disorder, a person must have experienced a manic episode at least once in his life; although major depressive episodes are common in bipolar disorder, they are not required for a diagnosis (APA, 2013). According to the DSM-5, a manic episode is characterized as a “distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased activity or energy lasting at least one week,” that lasts most of the time each day (APA, 2013, p. 124). During a manic episode, some experience a mood that is almost euphoric and become excessively talkative, sometimes spontaneously starting conversations with strangers; others become excessively irritable and complain or make hostile comments. The person may talk loudly and rapidly, exhibiting flight of ideas, abruptly switching from one topic to another. These individuals are easily distracted, which can make a conversation very difficult. They may exhibit grandiosity, in which they experience inflated but unjustified self-esteem and self-confidence. For example, they might quit a job in order to “strike it rich” in the stock market, despite lacking the knowledge, experience, and capital for such an endeavor. They may take on several tasks at the same time (e.g., several time-consuming projects at work) and yet show little, if any, need for sleep; some may go for days without sleep. Patients may also recklessly engage in pleasurable activities that could have harmful consequences, including spending sprees, reckless driving, making foolish investments, excessive gambling, or engaging in sexual encounters with strangers (APA, 2013).
During a manic episode, individuals usually feel as though they are not ill and do not need treatment. However, the reckless behaviors that often accompany these episodes—which can be antisocial, illegal, or physically threatening to others—may require involuntary hospitalization (APA, 2013). Some patients with bipolar disorder will experience a rapid-cycling subtype, which is characterized by at least four manic episodes (or some combination of at least four manic and major depressive episodes) within one year.
Risk Factors for Bipolar Disorder
Bipolar disorder is considerably less frequent than major depressive disorder. In the United States, 1 out of every 167 people meets the criteria for bipolar disorder each year, and 1 out of 100 meet the criteria within their lifetime (Merikangas et al., 2011). The rates are higher in men than in women, and about half of those with this disorder report onset before the age of 25 (Merikangas et al., 2011). Around 90% of those with bipolar disorder have a comorbid disorder, most often an anxiety disorder or a substance abuse problem. Unfortunately, close to half of the people suffering from bipolar disorder do not receive treatment (Merikangas & Tohen, 2011). Suicide rates are extremely high among those with bipolar disorder: around 36% of individuals with this disorder attempt suicide at least once in their lifetime (Novick, Swartz, & Frank, 2010), and between 15%–19% complete suicide (Newman, 2004).
The Biological Basis of Mood Disorders
Mood disorders have been shown to have a strong genetic and biological basis. Relatives of those with major depressive disorder have double the risk of developing major depressive disorder, whereas relatives of patients with bipolar disorder have over nine times the risk (Merikangas et al., 2011). The rate of concordance for major depressive disorder is higher among identical twins than fraternal twins (50% vs. 38%, respectively), as is that of bipolar disorder (67% vs. 16%, respectively), suggesting that genetic factors play a stronger role in bipolar disorder than in major depressive disorder (Merikangas et al. 2011).
People with mood disorders often have imbalances in certain neurotransmitters, particularly norepinephrine and serotonin (Thase, 2009). These neurotransmitters are important regulators of the bodily functions that are disrupted in mood disorders, including appetite, sex drive, sleep, arousal, and mood. Medications that are used to treat major depressive disorder typically boost serotonin and norepinephrine activity, whereas lithium—used in the treatment of bipolar disorder—blocks norepinephrine activity at the synapses (Figure 15.16).
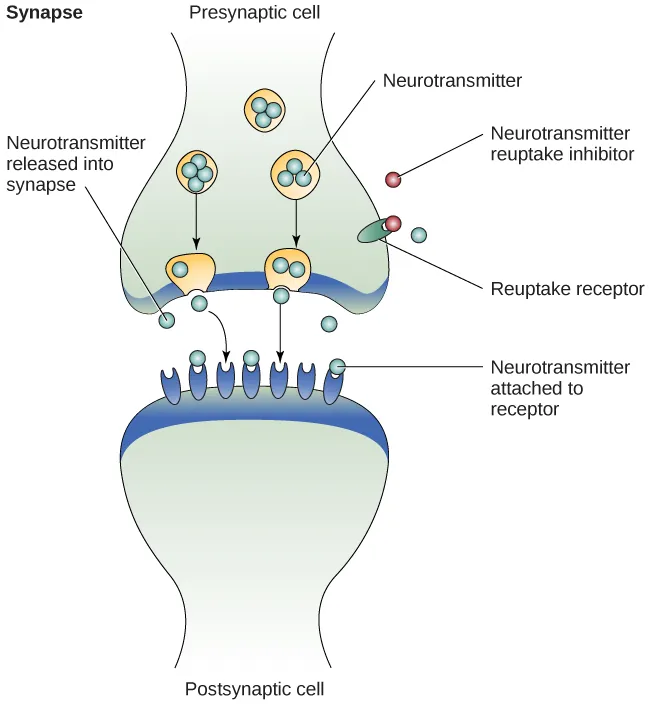
Depression is linked to abnormal activity in several regions of the brain (Fitzgerald, Laird, Maller, & Daskalakis, 2008) including those important in assessing the emotional significance of stimuli and experiencing emotions (amygdala), and in regulating and controlling emotions (like the prefrontal cortex, or PFC) (LeMoult, Castonguay, Joormann, & McAleavey, 2013). Depressed individuals show elevated amygdala activity (Drevets, Bogers, & Raichle, 2002), especially when presented with negative emotional stimuli, such as photos of sad faces (Figure 15.17) (Surguladze et al., 2005). Interestingly, heightened amygdala activation to negative emotional stimuli among depressed persons occurs even when stimuli are presented outside of conscious awareness (Victor, Furey, Fromm, Öhman, & Drevets, 2010), and it persists even after the negative emotional stimuli are no longer present (Siegle, Thompson, Carter, Steinhauer, & Thase, 2007). Additionally, depressed individuals exhibit less activation in the prefrontal, particularly on the left side (Davidson, Pizzagalli, & Nitschke, 2009). Because the PFC can dampen amygdala activation, thereby enabling one to suppress negative emotions (Phan et al., 2005), decreased activation in certain regions of the PFC may inhibit its ability to override negative emotions that might then lead to more negative mood states (Davidson et al., 2009). These findings suggest that depressed persons are more prone to react to emotionally negative stimuli, yet have greater difficulty controlling these reactions.
Since the 1950s, researchers have noted that depressed individuals have abnormal levels of cortisol, a stress hormone released into the blood by the neuroendocrine system during times of stress (Mackin & Young, 2004). When cortisol is released, the body initiates a fight-or-flight response in reaction to a threat or danger. Many people with depression show elevated cortisol levels (Holsboer & Ising, 2010), especially those reporting a history of early life trauma such as the loss of a parent or abuse during childhood (Baes, Tofoli, Martins, & Juruena, 2012). Such findings raise the question of whether high cortisol levels are a cause or a consequence of depression. High levels of cortisol are a risk factor for future depression (Halligan, Herbert, Goodyer, & Murray, 2007), and cortisol activates activity in the amygdala while deactivating activity in the PFC (McEwen, 2005)—both brain disturbances are connected to depression. Thus, high cortisol levels may have a causal effect on depression, as well as on its brain function abnormalities (van Praag, 2005). Also, because stress results in increased cortisol release (Michaud, Matheson, Kelly, Anisman, 2008), it is equally reasonable to assume that stress may precipitate depression.
A Diathesis-Stress Model and Major Depressive Disorders
Indeed, it has long been believed that stressful life events can trigger depression, and research has consistently supported this conclusion (Mazure, 1998). Stressful life events include significant losses, such as death of a loved one, divorce or separation, and serious health and money problems; life events such as these often precede the onset of depressive episodes (Brown & Harris, 1989). In particular, exit events—instances in which an important person departs (e.g., a death, divorce or separation, or a family member leaving home)—often occur prior to an episode (Paykel, 2003). Exit events are especially likely to trigger depression if these happenings occur in a way that humiliates or devalues the individual. For example, people who experience the breakup of a relationship initiated by the other person develop major depressive disorder at a rate more than 2 times that of people who experience the death of a loved one (Kendler, Hettema, Butera, Gardner, & Prescott, 2003).
Likewise, individuals who are exposed to traumatic stress during childhood—such as separation from a parent, family turmoil, and maltreatment (physical or sexual abuse)—are at a heightened risk of developing depression at any point in their lives (Kessler, 1997). A recent review of 16 studies involving over 23,000 subjects concluded that those who experience childhood maltreatment are more than 2 times as likely to develop recurring and persistent depression (Nanni, Uher, & Danese, 2012).
Of course, not everyone who experiences stressful life events or childhood adversities succumbs to depression—indeed, most do not. Clearly, a diathesis-stress interpretation of major depressive disorder, in which certain predispositions or vulnerability factors influence one’s reaction to stress, would seem logical. If so, what might such predispositions be? A study by Caspi and others (2003) suggests that an alteration in a specific gene that regulates serotonin (the 5-HTTLPR gene) might be one culprit. These investigators found that people who experienced several stressful life events were significantly more likely to experience episodes of major depression if they carried one or two short versions of this gene than if they carried two long versions. Those who carried one or two short versions of the 5-HTTLPR gene were unlikely to experience an episode, however, if they had experienced few or no stressful life events. Numerous studies have replicated these findings, including studies of people who experienced maltreatment during childhood (Goodman & Brand, 2009). In a recent investigation conducted in the United Kingdom (Brown & Harris, 2013), researchers found that childhood maltreatment before age 9 elevated the risk of chronic adult depression (a depression episode lasting for at least 12 months) among those individuals having one (LS) or two (SS) short versions of the 5-HTTLPR gene (Figure 15.18). Childhood maltreatment did not increase the risk for chronic depression for those have two long (LL) versions of this gene. Thus, genetic vulnerability may be one mechanism through which stress potentially leads to depression.
Cognitive Theories of Depression
Cognitive theories of depression take the view that depression is triggered by negative thoughts, interpretations, self-evaluations, and expectations (Joormann, 2009). These diathesis-stress models propose that depression is triggered by a “cognitive vulnerability” (negative and maladaptive thinking) and by precipitating stressful life events (Gotlib & Joormann, 2010). Perhaps the most well-known cognitive theory of depression was developed in the 1960s by psychiatrist Aaron Beck, based on clinical observations and supported by research (Beck, 2008). Beck theorized that depression-prone people possess depressive schemas, or mental predispositions to think about most things in a negative way (Beck, 1976). Depressive schemas contain themes of loss, failure, rejection, worthlessness, and inadequacy, and may develop early in childhood in response to adverse experiences, then remain dormant until they are activated by stressful or negative life events. Depressive schemas prompt dysfunctional and pessimistic thoughts about the self, the world, and the future. Beck believed that this dysfunctional style of thinking is maintained by cognitive biases, or errors in how we process information about ourselves, which lead us to focus on negative aspects of experiences, interpret things negatively, and block positive memories (Beck, 2008). A person whose depressive schema consists of a theme of rejection might be overly attentive to social cues of rejection (more likely to notice another’s frown), and he might interpret this cue as a sign of rejection and automatically remember past incidents of rejection. Longitudinal studies have supported Beck’s theory, in showing that a preexisting tendency to engage in this negative, self-defeating style of thinking—when combined with life stress—over time predicts the onset of depression (Dozois & Beck, 2008). Cognitive therapies for depression, aimed at changing a depressed person’s negative thinking, were developed as an expansion of this theory (Beck, 1976).
Another cognitive theory of depression, hopelessness theory, postulates that a particular style of negative thinking leads to a sense of hopelessness, which then leads to depression (Abramson, Metalsky, & Alloy, 1989). According to this theory, hopelessness is an expectation that unpleasant outcomes will occur or that desired outcomes will not occur, and there is nothing one can do to prevent such outcomes. A key assumption of this theory is that hopelessness stems from a tendency to perceive negative life events as having stable (“It’s never going to change”) and global (“It’s going to affect my whole life”) causes, in contrast to unstable (“It’s fixable”) and specific (“It applies only to this particular situation”) causes, especially if these negative life events occur in important life realms, such as relationships, academic achievement, and the like. Suppose a student who wishes to go to law school does poorly on an admissions test. If the student infers negative life events as having stable and global causes, she may believe that her poor performance has a stable and global cause (“I lack intelligence, and it’s going to prevent me from ever finding a meaningful career”), as opposed to an unstable and specific cause (“I was sick the day of the exam, so my low score was a fluke”). Hopelessness theory predicts that people who exhibit this cognitive style in response to undesirable life events will view such events as having negative implications for their future and self-worth, thereby increasing the likelihood of hopelessness—the primary cause of depression (Abramson et al., 1989). One study testing hopelessness theory measured the tendency to make negative inferences for bad life effects in participants who were experiencing uncontrollable stressors. Over the ensuing six months, those with scores reflecting high cognitive vulnerability were 7 times more likely to develop depression compared to those with lower scores (Kleim, Gonzalo, & Ehlers, 2011).
A third cognitive theory of depression focuses on how people’s thoughts about their distressed moods—depressed symptoms in particular—can increase the risk and duration of depression. This theory, which focuses on rumination in the development of depression, was first described in the late 1980s to explain the higher rates of depression in women than in men (Nolen-Hoeksema, 1987). Rumination is the repetitive and passive focus on the fact that one is depressed and dwelling on depressed symptoms, rather that distracting one’s self from the symptoms or attempting to address them in an active, problem-solving manner (Nolen-Hoeksema, 1991). When people ruminate, they have thoughts such as “Why am I so unmotivated? I just can’t get going. I’m never going to get my work done feeling this way” (Nolen-Hoeksema & Hilt, 2009, p. 393). Women are more likely than men to ruminate when they are sad or depressed (Butler & Nolen-Hoeksema, 1994), and the tendency to ruminate is associated with increases in depression symptoms (Nolen-Hoeksema, Larson, & Grayson, 1999), heightened risk of major depressive episodes (Abela & Hankin, 2011), and chronicity of such episodes (Robinson & Alloy, 2003)
Suicide
For some people with mood disorders, the extreme emotional pain they experience becomes unendurable. Overwhelmed by hopelessness, devastated by incapacitating feelings of worthlessness, and burdened with the inability to adequately cope with such feelings, they may consider suicide to be a reasonable way out. Suicide, defined by the CDC as “death caused by self-directed injurious behavior with any intent to die as the result of the behavior” (CDC, 2013a), in a sense represents an outcome of several things going wrong all at the same time (Crosby, Ortega, & Melanson, 2011). Not only must the person be biologically or psychologically vulnerable, but he must also have the means to perform the suicidal act, and he must lack the necessary protective factors (e.g., social support from friends and family, religion, coping skills, and problem-solving skills) that provide comfort and enable one to cope during times of crisis or great psychological pain (Berman, 2009).
Suicide is not listed as a disorder in the DSM-5; however, suffering from a mental disorder—especially a mood disorder—poses the greatest risk for suicide. Around 90% of those who complete suicides have a diagnosis of at least one mental disorder, with mood disorders being the most frequent (Fleischman, Bertolote, Belfer, & Beautrais, 2005). In fact, the association between major depressive disorder and suicide is so strong that one of the criteria for the disorder is thoughts of suicide, as discussed above (APA, 2013).
Suicide rates can be difficult to interpret because some deaths that appear to be accidental may in fact be acts of suicide (e.g., automobile crash). Nevertheless, investigations into U.S. suicide rates have uncovered these facts:
- Suicide was the 10th leading cause of death for all ages in 2010 (Centers for Disease Control and Prevention [CDC], 2012).
- There were 38,364 suicides in 2010 in the United States—an average of 105 each day (CDC, 2012).
- Suicide among males is 4 times higher than among females and accounts for 79% of all suicides; firearms are the most commonly used method of suicide for males, whereas poisoning is the most commonly used method for females (CDC, 2012).
- From 1991 to 2003, suicide rates were consistently higher among those 65 years and older. Since 2001, however, suicide rates among those ages 25–64 have risen consistently, and, since 2006, suicide rates have been greater for those ages 65 and older (CDC, 2013b). This increase in suicide rates among middle-aged Americans has prompted concern in some quarters that baby boomers (individuals born between 1946–1964) who face economic worry and easy access to prescription medication may be particularly vulnerable to suicide (Parker-Pope, 2013).
- The highest rates of suicide within the United States are among American Indians/Alaskan natives and Non-Hispanic Whites (CDC, 2013b).
- Suicide rates vary across the United States, with the highest rates consistently found in the mountain states of the west (Alaska, Montana, Nevada, Wyoming, Colorado, and Idaho) (Berman, 2009).
Contrary to popular belief, suicide rates peak during the springtime (April and May), not during the holiday season or winter. In fact, suicide rates are generally lowest during the winter months (Postolache et al., 2010).
Risk Factors For Suicide
Suicidal risk is especially high among people with substance abuse problems. Individuals with alcohol dependence are at 10 times greater risk for suicide than the general population (Wilcox, Conner, & Caine, 2004). The risk of suicidal behavior is especially high among those who have made a prior suicide attempt. Among those who attempt suicide, 16% make another attempt within a year and over 21% make another attempt within four years (Owens, Horrocks, & House, 2002). Suicidal individuals may be at high risk for terminating their life if they have a lethal means in which to act, such as a firearm in the home (Brent & Bridge, 2003). Withdrawal from social relationships, feeling as though one is a burden to others, and engaging in reckless and risk-taking behaviors may be precursors to suicidal behavior (Berman, 2009). A sense of entrapment or feeling unable to escape one’s miserable feelings or external circumstances (e.g., an abusive relationship with no perceived way out) predicts suicidal behavior (O’Connor, Smyth, Ferguson, Ryan, & Williams, 2013). Tragically, reports of suicides among adolescents following instances of cyberbullying have emerged in recent years. In one widely-publicized case a few years ago, Phoebe Prince, a 15-year-old Massachusetts high school student, committed suicide following incessant harassment and taunting from her classmates via texting and Facebook (McCabe, 2010).
Suicides can have a contagious effect on people. For example, another’s suicide, especially that of a family member, heightens one’s risk of suicide (Agerbo, Nordentoft, & Mortensen, 2002). Additionally, widely-publicized suicides tend to trigger copycat suicides in some individuals. One study examining suicide statistics in the United States from 1947–1967 found that the rates of suicide skyrocketed for the first month after a suicide story was printed on the front page of the New York Times (Phillips, 1974). Austrian researchers found a significant increase in the number of suicides by firearms in the three weeks following extensive reports in Austria’s largest newspaper of a celebrity suicide by gun (Etzersdorfer, Voracek, & Sonneck, 2004). A review of 42 studies concluded that media coverage of celebrity suicides is more than 14 times more likely to trigger copycat suicides than is coverage of non-celebrity suicides (Stack, 2000). This review also demonstrated that the medium of coverage is important: televised stories are considerably less likely to prompt a surge in suicides than are newspaper stories. Research suggests that a trend appears to be emerging whereby people use online social media to leave suicide notes, although it is not clear to what extent suicide notes on such media might induce copycat suicides (Ruder, Hatch, Ampanozi, Thali, & Fischer, 2011). Nevertheless, it is reasonable to conjecture that suicide notes left by individuals on social media may influence the decisions of other vulnerable people who encounter them (Luxton, June, & Fairall, 2012).
One possible contributing factor in suicide is brain chemistry. Contemporary neurological research shows that disturbances in the functioning of serotonin are linked to suicidal behavior (Pompili et al., 2010). Low levels of serotonin predict future suicide attempts and suicide completions, and low levels have been observed post-mortem among suicide victims (Mann, 2003). Serotonin dysfunction, as noted earlier, is also known to play an important role in depression; low levels of serotonin have also been linked to aggression and impulsivity (Stanley et al., 2000). The combination of these three characteristics constitutes a potential formula for suicide—especially violent suicide. A classic study conducted during the 1970s found that patients with major depressive disorder who had very low levels of serotonin attempted suicide more frequently and more violently than did patients with higher levels (Asberg, Thorén, Träskman, Bertilsson, & Ringberger, 1976; Mann, 2003).
Suicidal thoughts, plans, and even off-hand remarks (“I might kill myself this afternoon”) should always be taken extremely seriously. People who contemplate terminating their life need immediate help. Below are links to two excellent websites that contain resources (including hotlines) for people who are struggling with suicidal ideation, have loved ones who may be suicidal, or who have lost loved ones to suicide: http://www.afsp.org and http://suicidology.org.
IF YOU ARE IN CRISIS: 988 has been designated as the new three-digit dialing code that will route callers to the National Suicide Prevention Lifeline (now known as the 988 Suicide & Crisis Lifeline), and is now active across the United States.
When people call, text, or chat 988, they will be connected to trained counselors that are part of the existing Lifeline network. These trained counselors will listen, understand how their problems are affecting them, provide support, and connect them to resources if necessary.
The previous Lifeline phone number (1-800-273-8255) will always remain available to people in emotional distress or suicidal crisis.
The Lifeline’s network of over 200 crisis centers has been in operation since 2005, and has been proven to be effective. It’s the counselors at these local crisis centers who answer the contacts the Lifeline receives every day. Numerous studies have shown that callers feel less suicidal, less depressed, less overwhelmed and more hopeful after speaking with a Lifeline counselor.
15.7 Schizophrenia
Learning Objectives
By the end of this section, you will be able to:
- Recognize the essential nature of schizophrenia, avoiding the misconception that it involves a split personality
- Categorize and describe the major symptoms of schizophrenia
- Understand the interplay between genetic, biological, and environmental factors that are associated with the development of schizophrenia
- Discuss the importance of research examining prodromal symptoms of schizophrenia
Schizophrenia is a psychological disorder that is characterized by major disturbances in thought, perception, emotion, and behavior. About 1% of the population experiences schizophrenia in their lifetime, and usually the disorder is first diagnosed during early adulthood (early to mid-20s). Most people with schizophrenia experience significant difficulties in many day-to-day activities, such as holding a job, paying bills, caring for oneself (grooming and hygiene), and maintaining relationships with others. Frequent hospitalizations are more often the rule rather than the exception with schizophrenia. Even when they receive the best treatments available, many with schizophrenia will continue to experience serious social and occupational impairment throughout their lives.
What is schizophrenia? First, schizophrenia is not a condition involving a split personality; that is, schizophrenia is not the same thing as dissociative identity disorder (better known as multiple personality disorder). These disorders are sometimes confused because the word schizophrenia first coined by the Swiss psychiatrist Eugen Bleuler in 1911, derives from Greek words that refer to a “splitting” (schizo) of psychic functions (phrene) (Green, 2001).
Schizophrenia is considered a psychotic disorder, or one in which the person’s thoughts, perceptions, and behaviors are impaired to the point where they are not able to function normally in life. In informal terms, one who suffers from a psychotic disorder (that is, has a psychosis) is disconnected from the world in which most of us live.
Symptoms of Schizophrenia
The main symptoms of schizophrenia include hallucinations, delusions, disorganized thinking, disorganized or abnormal motor behavior, and negative symptoms (APA, 2013). A hallucination is a perceptual experience that occurs in the absence of external stimulation. Auditory hallucinations (hearing voices) occur in roughly two-thirds of patients with schizophrenia and are by far the most common form of hallucination (Andreasen, 1987). The voices may be familiar or unfamiliar, they may have a conversation or argue, or the voices may provide a running commentary on the person’s behavior (Tsuang, Farone, & Green, 1999).
Less common are visual hallucinations (seeing things that are not there) and olfactory hallucinations (smelling odors that are not actually present).
Delusions are beliefs that are contrary to reality and are firmly held even in the face of contradictory evidence. Many of us hold beliefs that some would consider odd, but a delusion is easily identified because it is clearly absurd. A person with schizophrenia may believe that their mother is plotting with the FBI to poison their coffee, or that their neighbor is an enemy spy who wants to kill them. These kinds of delusions are known as paranoid delusions, which involve the (false) belief that other people or agencies are plotting to harm the person. People with schizophrenia also may hold grandiose delusions, beliefs that one holds special power, unique knowledge, or is extremely important. For example, the person who claims to be Jesus Christ, or who claims to have knowledge going back 5,000 years, or who claims to be a great philosopher is experiencing grandiose delusions. Other delusions include the belief that one’s thoughts are being removed (thought withdrawal) or thoughts have been placed inside one’s head (thought insertion). Another type of delusion is somatic delusion, which is the belief that something highly abnormal is happening to one’s body (e.g., that one’s kidneys are being eaten by cockroaches).
Disorganized thinking refers to disjointed and incoherent thought processes—usually detected by what a person says. The person might ramble, exhibit loose associations (jump from topic to topic), or talk in a way that is so disorganized and incomprehensible that it seems as though the person is randomly cDisorganized thinkingombining words. Disorganized thinking is also exhibited by blatantly illogical remarks (e.g., “Fenway Park is in Boston. I live in Boston. Therefore, I live at Fenway Park.”) and by tangentiality: responding to others’ statements or questions by remarks that are either barely related or unrelated to what was said or asked. For example, if a person diagnosed with schizophrenia is asked if they are interested in receiving special job training, they might state that they once rode on a train somewhere. To a person with schizophrenia, the tangential (slightly related) connection between job training and riding a train are sufficient enough to cause such a response.
Disorganized or abnormal motor behavior refers to unusual behaviors and movements: becoming unusually active, exhibiting silly child-like behaviors (giggling and self-absorbed smiling), engaging in repeated and purposeless movements, or displaying odd facial exprcatatonic behaviorsessions and gestures. In some cases, the person will exhibit catatonic behaviors, which show decreased reactivity to the environment, such as posturing, in which the person maintains a rigid and bizarre posture for long periods of time, or catatonic stupor, a complete lack of movement and verbal behavior.
Negative symptoms are those that reflect noticeable decreases and absences in certain behaviors, emotions, or drives (Green, 2001). A person who exhibits diminished emotional expression shows no emotion in their facial expressions, speech, or movements, even when such expressions are normal or expected. Avolition is characterized by a lack of motivation to engage in self-initiated and meaningful activity, including the most basic of tasks, such as bathing and grooming. Alogia refers to reduced speech output; in simple terms, patients do not say much. Another negative symptom is asociality, or social withdrawal and lack of interest in engaging in social interactions with others. A final negative symptom, anhedonia, refers to an inability to experience pleasure. One who exhibits anhedonia expresses little interest in what most people consider to be pleasurable activities, such as hobbies, recreation, or sexual activity.
Causes of Schizophrenia
There is considerable evidence suggesting that schizophrenia has a genetic basis. The risk of developing schizophrenia is nearly 6 times greater if one has a parent with schizophrenia than if one does not (Goldstein, Buka, Seidman, & Tsuang, 2010). Additionally, one’s risk of developing schizophrenia increases as genetic relatedness to family members diagnosed with schizophrenia increases (Gottesman, 2001).
Genes
When considering the role of genetics in schizophrenia, as in any disorder, conclusions based on family and twin studies are subject to criticism. This is because family members who are closely related (such as siblings) are more likely to share similar environments than are family members who are less closely related (such as cousins); further, identical twins may be more likely to be treated similarly by others than might fraternal twins. Thus, family and twin studies cannot completely rule out the possible effects of shared environments and experiences. Such problems can be corrected by using adoption studies, in which children are separated from their parents at an early age. One of the first adoption studies of schizophrenia conducted by Heston (1966) followed 97 adoptees, including 47 who were born to mothers with schizophrenia, over a 36-year period. Five of the 47 adoptees (11%) whose mothers had schizophrenia were later diagnosed with schizophrenia, compared to none of the 50 control adoptees. Other adoption studies have consistently reported that for adoptees who are later diagnosed with schizophrenia, their biological relatives have a higher risk of schizophrenia than do adoptive relatives (Shih, Belmonte, & Zandi, 2004).
Although adoption studies have supported the hypothesis that genetic factors contribute to schizophrenia, they have also demonstrated that the disorder most likely arises from a combination of genetic and environmental factors, rather than just genes themselves. For example, investigators in one study examined the rates of schizophrenia among 303 adoptees (Tienari et al., 2004). A total of 145 of the adoptees had biological mothers with schizophrenia; these adoptees constituted the high genetic risk group. The other 158 adoptees had mothers with no psychiatric history; these adoptees composed the low genetic risk group. The researchers managed to determine whether the adoptees’ families were either healthy or disturbed. For example, the adoptees were considered to be raised in a disturbed family environment if the family exhibited a lot of criticism, conflict, and a lack of problem-solving skills. The findings revealed that adoptees whose biological mothers had schizophrenia (high genetic risk) and who had been raised in a disturbed family environment were much more likely to develop schizophrenia or another psychotic disorder (36.8%) than were adoptees whose biological mothers had schizophrenia but who had been raised in a healthy environment (5.8%), or than adoptees with a low genetic risk who were raised in either a disturbed (5.3%) or healthy (4.8%) environment. Because the adoptees who were at high genetic risk were likely to develop schizophrenia only if they were raised in a disturbed home environment, this study supports a diathesis-stress interpretation of schizophrenia—both genetic vulnerability and environmental stress are necessary for schizophrenia to develop, genes alone do not show the complete picture.
Neurotransmitters
If we accept that schizophrenia is at least partly genetic in origin, as it seems to be, it makes sense that the next step should be to identify biological abnormalities commonly found in people with the disorder. Perhaps not surprisingly, a number of neurobiological factors have indeed been found to be related to schizophrenia. One such factor that has received considerable attention for many years is the neurotransmitter dopamine. Interest in the role of dopamine in schizophrenia was stimulated by two sets of findings: drugs that increase dopamine levels can produce schizophrenia-like symptoms, and medications that block dopamine activity reduce the symptoms (Howes & Kapur, 2009). The dopamine hypothesis of schizophrenia proposed that an overabundance of dopamine or too many dopamine receptors are responsible for the onset and maintenance of schizophrenia (Snyder, 1976). More recent work in this area suggests that abnormalities in dopamine vary by brain region and thus contribute to symptoms in unique ways. In general, this research has suggested that an overabundance of dopamine in the limbic system may be responsible for some symptoms, such as hallucinations and delusions, whereas low levels of dopamine in the prefrontal cortex might be responsible primarily for the negative symptoms (avolition, alogia, asociality, and anhedonia) (Davis, Kahn, Ko, & Davidson, 1991). In recent years, serotonin has received attention, and newer antipsychotic medications used to treat the disorder work by blocking serotonin receptors (Baumeister & Hawkins, 2004).
Brain Anatomy
Brain imaging studies reveal that people with schizophrenia have enlarged ventricles, the cavities within the brain that contain cerebral spinal fluid (Green, 2001). This finding is important because larger than normal ventricles suggests that various brain regions are reduced in size, thus implying that schizophrenia is associated with a loss of brain tissue. In addition, many people with schizophrenia display a reduction in gray matter (cell bodies of neurons) in the frontal lobes (Lawrie & Abukmeil, 1998), and many show less frontal lobe activity when performing cognitive tasks (Buchsbaum et al., 1990). The frontal lobes are important in a variety of complex cognitive functions, such as planning and executing behavior, attention, speech, movement, and problem solving. Hence, abnormalities in this region provide merit in explaining why people with schizophrenia experience deficits in these of areas.
Events During Pregnancy
Why do people with schizophrenia have these brain abnormalities? A number of environmental factors that could impact normal brain development might be at fault. High rates of obstetric complications in the births of children who later developed schizophrenia have been reported (Cannon, Jones, & Murray, 2002). In addition, people are at an increased risk for developing schizophrenia if their mother was exposed to influenza during the first trimester of pregnancy (Brown et al., 2004). Research has also suggested that a person’s emotional stress during pregnancy may increase the risk of schizophrenia in offspring. One study reported that the risk of schizophrenia is elevated substantially in offspring whose mothers experienced the death of a relative during the first trimester of pregnancy (Khashan et al., 2008).
Marijuana
Another variable that is linked to schizophrenia is marijuana use. Although a number of reports have shown that individuals with schizophrenia are more likely to use marijuana than are individuals without schizophrenia (Thornicroft, 1990), such investigations cannot determine if marijuana use leads to schizophrenia, or vice versa. However, a number of longitudinal studies have suggested that marijuana use is, in fact, a risk factor for schizophrenia. A classic investigation of over 45,000 Swedish military personnel who were followed up after 15 years found that those individuals who had reported using marijuana at least once by the time they were conscripted (drafted) into the military were more than 2 times as likely to develop schizophrenia during the ensuing 15 years than were those who reported never using marijuana; those who had indicated using marijuana 50 or more times were 6 times as likely to develop schizophrenia (Andréasson, Allbeck, Engström, & Rydberg, 1987). More recently, a review of 35 longitudinal studies found a substantially increased risk of schizophrenia and other psychotic disorders in people who had used marijuana, with the greatest risk in the most frequent users (Moore et al., 2007). Other work has found that marijuana use is associated with an onset of psychotic disorders at an earlier age (Large, Sharma, Compton, Slade, & Nielssen, 2011). Overall, the available evidence seems to indicate that marijuana use plays a causal role in the development of schizophrenia, although it is important to point out that marijuana use is not an essential or sufficient risk factor as not all people with schizophrenia have used marijuana and the majority of marijuana users do not develop schizophrenia (Casadio, Fernandes, Murray, & Di Forti, 2011). One plausible interpretation of the data is that early marijuana use may disrupt normal brain development during important early maturation periods in adolescence (Trezza, Cuomo, & Vanderschuren, 2008). Thus, early marijuana use may set the stage for the development of schizophrenia and other psychotic disorders, especially among individuals with an established vulnerability (Casadio et al., 2011).
Schizophrenia: Early Warning Signs
Early detection and treatment of conditions such as heart disease and cancer have improved survival rates and quality of life for people who suffer from these conditions. A new approach involves identifying people who show minor symptoms of psychosis, such as unusual thought content, paranoia, odd communication, delusions, problems at school or work, and a decline in social functioning—which are coined prodromal symptoms—and following these individuals over time to determine which of them develop a psychotic disorder and which factors best predict such a disorder. A number of factors have been identified that predict a greater likelihood that prodromal individuals will develop a psychotic disorder: genetic risk (a family history of psychosis), recent deterioration in functioning, high levels of unusual thought content, high levels of suspicion or paranoia, poor social functioning, and a history of substance abuse (Fusar-Poli et al., 2013). Further research will enable a more accurate prediction of those at greatest risk for developing schizophrenia, and thus to whom early intervention efforts should be directed.
DIG DEEPER: Forensic Psychology
In August 2013, 17-year-old Cody Metzker-Madsen attacked 5-year-old Dominic Elkins on his foster parents’ property. Believing that he was fighting goblins and that Dominic was the goblin commander, Metzker-Madsen beat Dominic with a brick and then held him face down in a creek. Dr. Alan Goldstein, a clinical and forensic psychologist, testified that Metzker-Madsen believed that the goblins he saw were real and was not aware that it was Dominic at the time. He was found not guilty by reason of insanity and was not held legally responsible for Dominic’s death (Nelson, 2014). Cody was also found to be a danger to himself or others. He will be held in a psychiatric facility until he is judged to be no longer dangerous. This does not mean that he “got away with” anything. In fact, according to the American Psychiatric Association, individuals who are found not guilty by reason of insanity are often confined to psychiatric hospitals for as long or longer than they would have spent in prison for a conviction.
Most people with mental illness are not violent. Only 3–5% of violent acts are committed by individuals diagnosed with severe mental illness, whereas individuals with severe mental illnesses are more than ten times as likely to be victims of crime (MentalHealth.gov, 2017). The psychologists who work with individuals such as Metzker-Madsen are part of the subdiscipline of forensic psychology. Forensic psychologists are involved in psychological assessment and treatment of individuals involved with the legal system. They use their knowledge of human behavior and mental illness to assist the judicial and legal system in making decisions in cases involving such issues as personal injury suits, workers’ compensation, competency to stand trial, and pleas of not guilty by reason of insanity.
15.8 Dissociative Disorders
Learning Objectives
By the end of this section, you will be able to:
- Describe the essential nature of dissociative disorders
- Identify and differentiate the symptoms of dissociative amnesia, depersonalization/ derealization disorder, and dissociative identity disorder
- Discuss the potential role of both social and psychological factors in dissociative identity disorder
Dissociative disorders are characterized by an individual becoming split off, or dissociated, from her core sense of self. Memory and identity become disturbed; these disturbances have a psychological rather than physical cause. Dissociative disorders listed in the DSM-5 include dissociative amnesia, depersonalization/derealization disorder, and dissociative identity disorder.
Dissociative Amnesia
Amnesia refers to the partial or total forgetting of some experience or event. An individual with dissociative amnesia is unable to recall important personal information, usually following an extremely stressful or traumatic experience such as combat, natural disasters, or being the victim of violence. The memory impairments are not caused by ordinary forgetting. Some individuals with dissociative amnesia will also experience dissociative fugue (from the word “to flee” in French), whereby they suddenly wander away from their home, experience confusion about their identity, and sometimes even adopt a new identity (Cardeña & Gleaves, 2006). Most fugue episodes last only a few hours or days, but some can last longer. One study of residents in communities in upstate New York reported that about 1.8% experienced dissociative amnesia in the previous year (Johnson, Cohen, Kasen, & Brook, 2006).
Some have questioned the validity of dissociative amnesia (Pope, Hudson, Bodkin, & Oliva, 1998); it has even been characterized as a “piece of psychiatric folklore devoid of convincing empirical support” (McNally, 2003, p. 275). Notably, scientific publications regarding dissociative amnesia rose during the 1980s and reached a peak in the mid-1990s, followed by an equally sharp decline by 2003; in fact, only 13 cases of individuals with dissociative amnesia worldwide could be found in the literature that same year (Pope, Barry, Bodkin, & Hudson, 2006). Further, no description of individuals showing dissociative amnesia following a trauma exists in any fictional or nonfictional work prior to 1800 (Pope, Poliakoff, Parker, Boynes, & Hudson, 2006). However, a study of 82 individuals who enrolled for treatment at a psychiatric outpatient hospital found that nearly 10% met the criteria for dissociative amnesia, perhaps suggesting that the condition is underdiagnosed, especially in psychiatric populations (Foote, Smolin, Kaplan, Legatt, & Lipschitz, 2006).
Depersonalization/Derealization Disorder
Depersonalization/derealization disorder is characterized by recurring episodes of depersonalization, derealization, or both. Depersonalization is defined as feelings of “unreality or detachment from, or unfamiliarity with, one’s whole self or from aspects of the self” (APA, 2013, p. 302). Individuals who experience depersonalization might believe their thoughts and feelings are not their own; they may feel robotic as though they lack control over their movements and speech; they may experience a distorted sense of time and, in extreme cases, they may sense an “out-of-body” experience in which they see themselves from the vantage point of another person. Derealization is conceptualized as a sense of “unreality or detachment from, or unfamiliarity with, the world, be it individuals, inanimate objects, or all surroundings” (APA, 2013, p. 303). A person who experiences derealization might feel as though he is in a fog or a dream, or that the surrounding world is somehow artificial and unreal. Individuals with depersonalization/derealization disorder often have difficulty describing their symptoms and may think they are going crazy (APA, 2013).
Dissociative Identity Disorder
By far, the most well-known dissociative disorder is dissociative identity disorder (formerly called multiple personality disorder). People with dissociative identity disorder exhibit two or more separate personalities or identities, each well-defined and distinct from one another. They also experience memory gaps for the time during which another identity is in charge (e.g., one might find unfamiliar items in her shopping bags or among her possessions), and in some cases may report hearing voices, such as a child’s voice or the sound of somebody crying (APA, 2013). The study of upstate New York residents mentioned above (Johnson et al., 2006) reported that 1.5% of their sample experienced symptoms consistent with dissociative identity disorder in the previous year.
Dissociative identity disorder (DID) is highly controversial. Some believe that people fake symptoms to avoid the consequences of illegal actions (e.g., “I am not responsible for shoplifting because it was my other personality”). In fact, it has been demonstrated that people are generally skilled at adopting the role of a person with different personalities when they believe it might be advantageous to do so. As an example, Kenneth Bianchi was an infamous serial killer who, along with his cousin, murdered over a dozen females around Los Angeles in the late 1970s. Eventually, he and his cousin were apprehended. At Bianchi’s trial, he pled not guilty by reason of insanity, presenting himself as though he had DID and claiming that a different personality (“Steve Walker”) committed the murders. When these claims were scrutinized, he admitted faking the symptoms and was found guilty (Schwartz, 1981).
A second reason DID is controversial is because rates of the disorder suddenly skyrocketed in the 1980s. More cases of DID were identified during the five years prior to 1986 than in the preceding two centuries (Putnam, Guroff, Silberman, Barban, & Post, 1986). Although this increase may be due to the development of more sophisticated diagnostic techniques, it is also possible that the popularization of DID—helped in part by Sybil, a popular 1970s book (and later film) about a woman with 16 different personalities—may have prompted clinicians to overdiagnose the disorder (Piper & Merskey, 2004). Casting further scrutiny on the existence of multiple personalities or identities is the recent suggestion that the story of Sybil was largely fabricated, and the idea for the book might have been exaggerated (Nathan, 2011).
Despite its controversial nature, DID is clearly a legitimate and serious disorder, and although some people may fake symptoms, others suffer their entire lives with it. People with this disorder tend to report a history of childhood trauma, some cases having been corroborated through medical or legal records (Cardeña & Gleaves, 2006). Research by Ross et al. (1990) suggests that in one study about 95% of people with DID were physically and/or sexually abused as children. Of course, not all reports of childhood abuse can be expected to be valid or accurate. However, there is strong evidence that traumatic experiences can cause people to experience states of dissociation, suggesting that dissociative states—including the adoption of multiple personalities—may serve as a psychologically important coping mechanism for threat and danger (Dalenberg et al., 2012).
15.9 Developmental Disorders
Learning Objectives
By the end of this section, you will be able to:
- Describe the nature and symptoms of attention deficit/hyperactivity disorder and autism spectrum disorder
- Discuss the prevalence and factors that contribute to the development of these disorders
- Describe how genetics and environment affect intelligence
- Explain the relationship between IQ scores and socioeconomic status
- Describe the difference between a learning disability and a developmental disorder
Most of the disorders we have discussed so far are typically diagnosed in adulthood, although they can and sometimes do occur during childhood. However, there are a group of conditions that, when present, are diagnosed early in childhood, often before the time a child enters school. These conditions are listed in the DSM-5 as neurodevelopmental disorders, and they involve developmental problems in personal, social, academic, and intellectual functioning (APA, 2013). In this section, we will discuss two such disorders: attention deficit/ hyperactivity disorder and autism.
Attention Deficit/Hyperactivity Disorder
Diego is always active, from the time he wakes up in the morning until the time he goes to bed at night. His mother reports that he came out the womb kicking and screaming, and he has not stopped moving since. He has a sweet disposition, but always seems to be in trouble with his teachers, parents, and after-school program counselors. He seems to accidently break things; he lost his jacket three times last winter, and he never seems to sit still. His teachers believe he is a smart child, but he never finishes anything he starts and is so impulsive that he does not seem to learn much in school.
Diego likely has attention deficit/hyperactivity disorder (ADHD). The symptoms of this disorder were first described by Hans Hoffman in the 1920s. While taking care of his son while his wife was in the hospital giving birth to a second child, Hoffman noticed that the boy had trouble concentrating on his homework, had a short attention span, and had to repeatedly go over easy homework to learn the material (Jellinek & Herzog, 1999). Later, it was discovered that many hyperactive children—those who are fidgety, restless, socially disruptive, and have trouble with impulse control—also display short attention spans, problems with concentration, and distractibility. By the 1970s, it had become clear that many children who display attention problems often also exhibit signs of hyperactivity. In recognition of such findings, the DSM-III (published in 1980) included a new disorder: attention deficit disorder with and without hyperactivity, now known as attention deficit/hyperactivity disorder (ADHD).
A child with ADHD shows a constant pattern of inattention and/or hyperactive and impulsive behavior that interferes with normal functioning (APA, 2013). Some of the signs of inattention include great difficulty with and avoidance of tasks that require sustained attention (such as conversations or reading), failure to follow instructions (often resulting in failure to complete school work and other duties), disorganization (difficulty keeping things in order, poor time management, sloppy and messy work), lack of attention to detail, becoming easily distracted, and forgetfulness. Hyperactivity is characterized by excessive movement, and includes fidgeting or squirming, leaving one’s seat in situations when remaining seated is expected, having trouble sitting still (e.g., in a restaurant), running about and climbing on things, blurting out responses before another person’s question or statement has been completed, difficulty waiting one’s turn for something, and interrupting and intruding on others. Frequently, the hyperactive child comes across as noisy and boisterous. The child’s behavior is hasty, impulsive, and seems to occur without much forethought; these characteristics may explain why adolescents and young adults diagnosed with ADHD receive more traffic tickets and have more automobile accidents than do others (Thompson, Molina, Pelham, & Gnagy, 2007).
ADHD occurs in about 5% of children (APA, 2013). On the average, boys are 3 times more likely to have ADHD than are girls; however, such findings might reflect the greater propensity of boys to engage in aggressive and antisocial behavior and thus incur a greater likelihood of being referred to psychological clinics (Barkley, 2006). Children with ADHD face severe academic and social challenges. Compared to their non-ADHD counterparts, children with ADHD have lower grades and standardized test scores and higher rates of expulsion, grade retention, and dropping out (Loe & Feldman, 2007). they also are less well-liked and more often rejected by their peers (Hoza et al., 2005).
Previously, ADHD was thought to fade away by adolescence. However, longitudinal studies have suggested that ADHD is a chronic problem, one that can persist into adolescence and adulthood (Barkley, Fischer, Smallish, & Fletcher, 2002). A recent study found that 29.3% of adults who had been diagnosed with ADHD decades earlier still showed symptoms (Barbaresi et al., 2013). Somewhat troubling, this study also reported that nearly 81% of those whose ADHD persisted into adulthood had experienced at least one other comorbid disorder, compared to 47% of those whose ADHD did not persist.
Life Problems from ADHD
Children diagnosed with ADHD face considerably worse long-term outcomes than do those children who do not receive such a diagnosis. In one investigation, 135 adults who had been identified as having ADHD symptoms in the 1970s were contacted decades later and interviewed (Klein et al., 2012). Compared to a control sample of 136 participants who had never been diagnosed with ADHD, those who were diagnosed as children:
- had worse educational attainment (more likely to have dropped out of high school and less likely to have earned a bachelor’s degree);
- had lower socioeconomic status;
- held less prestigious occupational positions;
- were more likely to be unemployed;
- made considerably less in salary;
- scored worse on a measure of occupational functioning (indicating, for example, lower job satisfaction, poorer work relationships, and more firings);
- scored worse on a measure of social functioning (indicating, for example, fewer friendships and less involvement in social activities);
- were more likely to be divorced; and
- were more likely to have non-alcohol-related substance abuse problems. (Klein et al., 2012)
Longitudinal studies also show that children diagnosed with ADHD are at higher risk for substance abuse problems. One study reported that childhood ADHD predicted later drinking problems, daily smoking, and use of marijuana and other illicit drugs (Molina & Pelham, 2003). The risk of substance abuse problems appears to be even greater for those with ADHD who also exhibit antisocial tendencies (Marshal & Molina, 2006).
Causes of ADHD
Family and twin studies indicate that genetics play a significant role in the development of ADHD. Burt (2009), in a review of 26 studies, reported that the median rate of concordance for identical twins was .66 (one study reported a rate of .90), whereas the median concordance rate for fraternal twins was .20. This study also found that the median concordance rate for unrelated (adoptive) siblings was .09; although this number is small, it is greater than 0, thus suggesting that the environment may have at least some influence. Another review of studies concluded that the heritability of inattention and hyperactivity were 71% and 73%, respectively (Nikolas & Burt, 2010).
The specific genes involved in ADHD are thought to include at least two that are important in the regulation of the neurotransmitter dopamine (Gizer, Ficks, & Waldman, 2009), suggesting that dopamine may be important in ADHD. Indeed, medications used in the treatment of ADHD, such as methylphenidate (Ritalin) and amphetamine with dextroamphetamine (Adderall), have stimulant qualities and elevate dopamine activity. People with ADHD show less dopamine activity in key regions of the brain, especially those associated with motivation and reward (Volkow et al., 2009), which provides support to the theory that dopamine deficits may be a vital factor in the development this disorder (Swanson et al., 2007).
Brain imaging studies have shown that children with ADHD exhibit abnormalities in their frontal lobes, an area in which dopamine is in abundance. Compared to children without ADHD, those with ADHD appear to have smaller frontal lobe volume, and they show less frontal lobe activation when performing mental tasks. Recall that one of the functions of the frontal lobes is to inhibit our behavior. Thus, abnormalities in this region may go a long way toward explaining the hyperactive, uncontrolled behavior of ADHD.
By the 1970s, many had become aware of the connection between nutritional factors and childhood behavior. At the time, much of the public believed that hyperactivity was caused by sugar and food additives, such as artificial coloring and flavoring. Undoubtedly, part of the appeal of this hypothesis was that it provided a simple explanation of (and treatment for) behavioral problems in children. A statistical review of 16 studies, however, concluded that sugar consumption has no effect at all on the behavioral and cognitive performance of children (Wolraich, Wilson, & White, 1995). Additionally, although food additives have been shown to increase hyperactivity in non-ADHD children, the effect is rather small (McCann et al., 2007). Numerous studies, however, have shown a significant relationship between exposure to nicotine in cigarette smoke during the prenatal period and ADHD (Linnet et al., 2003). Maternal smoking during pregnancy is associated with the development of more severe symptoms of the disorder (Thakur et al., 2013).
Is ADHD caused by poor parenting? Not likely. Remember, the genetics studies discussed above suggested that the family environment does not seem to play much of a role in the development of this disorder; if it did, we would expect the concordance rates to be higher for fraternal twins and adoptive siblings than has been demonstrated. All things considered, the evidence seems to point to the conclusion that ADHD is triggered more by genetic and neurological factors and less by social or environmental ones.
DIG DEEPER: Why Is the Prevalence Rate of ADHD Increasing?
Many people believe that the rates of ADHD have increased in recent years, and there is evidence to support this contention. In a recent study, investigators found that the parent-reported prevalence of ADHD among children (4–17 years old) in the United States increased by 22% during a 4-year period, from 7.8% in 2003 to 9.5% in 2007 (CDC, 2010). Over time this increase in parent-reported ADHD was observed in all sociodemographic groups and was reflected by substantial increases in 12 states (Indiana, North Carolina, and Colorado were the top three). The increases were greatest for older teens (ages 15–17), multiracial and Hispanic children, and children with a primary language other than English. Another investigation found that from 1998–2000 through 2007–2009 the parent-reported prevalence of ADHD increased among U.S. children between the ages of 5–17 years old, from 6.9% to 9.0% (Akinbami, Liu, Pastor, & Reuben, 2011).
A major weakness of both studies was that children were not actually given a formal diagnosis. Instead, parents were simply asked whether or not a doctor or other health-care provider had ever told them their child had ADHD; the reported prevalence rates thus may have been affected by the accuracy of parental memory. Nevertheless, the findings from these studies raise important questions concerning what appears to be a demonstrable rise in the prevalence of ADHD. Although the reasons underlying this apparent increase in the rates of ADHD over time are poorly understood and, at best, speculative, several explanations are viable:
- ADHD may be over-diagnosed by doctors who are too quick to medicate children as a behavior treatment.
- There is greater awareness of ADHD now than in the past. Nearly everyone has heard of ADHD, and most parents and teachers are aware of its key symptoms. Thus, parents may be quick to take their children to a doctor if they believe their child possesses these symptoms, or teachers may be more likely now than in the past to notice the symptoms and refer the child for evaluation.
- The use of computers, video games, iPhones, and other electronic devices has become pervasive among children in the early 21st century, and these devices could potentially shorten children’s attentions spans. Thus, what might seem like inattention to some parents and teachers could simply reflect exposure to too much technology.
- ADHD diagnostic criteria have changed over time.
Autism Spectrum Disorder
A seminal paper published in 1943 by psychiatrist Leo Kanner described an unusual neurodevelopmental condition he observed in a group of children. He called this condition early infantile autism, and it was characterized mainly by an inability to form close emotional ties with others, speech and language abnormalities, repetitive behaviors, and an intolerance of minor changes in the environment and in normal routines (Bregman, 2005). What the DSM-5 refers to as autism spectrum disorder today, is a direct extension of Kanner’s work.
Autism spectrum disorder is probably the most misunderstood and puzzling of the neurodevelopmental disorders. Children with this disorder show signs of significant disturbances in three main areas: (a) deficits in social interaction, (b) deficits in communication, and (c) repetitive patterns of behavior or interests. These disturbances appear early in life and cause serious impairments in functioning (APA, 2013). The child with autism spectrum disorder might exhibit deficits in social interaction by not initiating conversations with other children or turning their head away when spoken to. Typically, these children do not make eye contact with others and seem to prefer playing alone rather than with others. In a certain sense, it is almost as though these individuals live in a personal and isolated social world others are simply not privy to or able to penetrate. Communication deficits can range from a complete lack of speech, to one word responses (e.g., saying “Yes” or “No” when replying to questions or statements that require additional elaboration), to echoed speech (e.g., parroting what another person says, either immediately or several hours or even days later), to difficulty maintaining a conversation because of an inability to reciprocate others’ comments. These deficits can also include problems in using and understanding nonverbal cues (e.g., facial expressions, gestures, and postures) that facilitate normal communication.
Repetitive patterns of behavior or interests can be exhibited a number of ways. The child might engage in stereotyped, repetitive movements (rocking, head-banging, or repeatedly dropping an object and then picking it up), or she might show great distress at small changes in routine or the environment. For example, the child might throw a temper tantrum if an object is not in its proper place or if a regularly-scheduled activity is rescheduled. In some cases, the person with autism spectrum disorder might show highly restricted and fixated interests that appear to be abnormal in their intensity. For instance, the person might learn and memorize every detail about something even though doing so serves no apparent purpose. Importantly, autism spectrum disorder is not the same thing as intellectual disability, although these two conditions are often comorbid. The DSM-5 specifies that the symptoms of autism spectrum disorder are not caused or explained by intellectual disability.
Life Problems From Autism Spectrum Disorder
Autism spectrum disorder is referred to in everyday language as autism; in fact, the disorder was termed “autistic disorder” in earlier editions of the DSM, and its diagnostic criteria were much narrower than those of autism spectrum disorder. The qualifier “spectrum” in autism spectrum disorder is used to indicate that individuals with the disorder can show a range, or spectrum, of symptoms that vary in their magnitude and severity: some severe, others less severe. The previous edition of the DSM included a diagnosis of Asperger’s disorder, generally recognized as a less severe form of autistic disorder; individuals diagnosed with Asperger’s disorder were described as having average or high intelligence and a strong vocabulary, but exhibiting impairments in social interaction and social communication, such as talking only about their special interests (Wing, Gould, & Gillberg, 2011). However, because research has failed to demonstrate that Asperger’s disorder differs qualitatively from autistic disorder, the DSM-5 does not include it, which is prompting concerns among some parents that their children may no longer be eligible for special services (“Asperger’s Syndrome Dropped,” 2012). Some individuals with autism spectrum disorder, particularly those with better language and intellectual skills, can live and work independently as adults. However, most do not because the symptoms remain sufficient to cause serious impairment in many realms of life (APA, 2013).
Current estimates from the Center for Disease Control and Prevention’s Autism and Developmental Disabilities Monitoring Network indicate that 1 in 59 children in the United States has autism spectrum disorder; the disorder is 4 times more common among boys (1 in 38) than in girls (1 in 152) (Baio et al, 2018). Rates of autistic spectrum disorder have increased dramatically since the 1980s. For example, California saw an increase of 273% in reported cases from 1987 through 1998 (Byrd, 2002); between 2000 and 2008, the rate of autism diagnoses in the United States increased 78% (CDC, 2012). Although it is difficult to interpret this increase, it is possible that the rise in prevalence is the result of the broadening of the diagnosis, increased efforts to identify cases in the community, and greater awareness and acceptance of the diagnosis. In addition, mental health professionals are now more knowledgeable about autism spectrum disorder and are better equipped to make the diagnosis, even in subtle cases (Novella, 2008).
Causes of Autism Spectrum Disorder
Early theories of autism placed the blame squarely on the shoulders of the child’s parents, particularly the mother. Bruno Bettelheim (an Austrian-born American child psychologist who was heavily influenced by Sigmund Freud’s ideas) suggested that a mother’s ambivalent attitudes and her frozen and rigid emotions toward her child were the main causal factors in childhood autism. In what must certainly stand as one of the more controversial assertions in psychology over the last 50 years, he wrote, “I state my belief that the precipitating factor in infantile autism is the parent’s wish that his child should not exist” (Bettelheim, 1967, p. 125). As you might imagine, Bettelheim did not endear himself to a lot of people with this position; incidentally, no scientific evidence exists supporting his claims.
The exact causes of autism spectrum disorder remain unknown despite massive research efforts over the last two decades (Meek, Lemery-Chalfant, Jahromi, & Valiente, 2013). Autism appears to be strongly influenced by genetics, as identical twins show concordance rates of 60%–90%, whereas concordance rates for fraternal twins and siblings are 5%–10% (Autism Genome Project Consortium, 2007). Many different genes and gene mutations have been implicated in autism (Meek et al., 2013). Among the genes involved are those important in the formation of synaptic circuits that facilitate communication between different areas of the brain (Gauthier et al., 2011). A number of environmental factors are also thought to be associated with increased risk for autism spectrum disorder, at least in part, because they contribute to new mutations. These factors include exposure to pollutants, such as plant emissions and mercury, urban versus rural residence, and vitamin D deficiency (Kinney, Barch, Chayka, Napoleon, & Munir, 2009).
Child Vaccinations and Autism Spectrum Disorder
In the late 1990s, a prestigious medical journal published an article purportedly showing that autism is triggered by the MMR (measles, mumps, and rubella) vaccine. These findings were very controversial and drew a great deal of attention, sparking an international forum on whether children should be vaccinated. In a shocking turn of events, some years later the article was retracted by the journal that had published it after accusations of fraud on the part of the lead researcher. Despite the retraction, the reporting in popular media led to concerns about a possible link between vaccines and autism persisting. A recent survey of parents, for example, found that roughly a third of respondents expressed such a concern (Kennedy, LaVail, Nowak, Basket, & Landry, 2011); and perhaps fearing that their children would develop autism, more than 10% of parents of young children refuse or delay vaccinations (Dempsey et al., 2011). Some parents of children with autism mounted a campaign against scientists who refuted the vaccine-autism link. Even politicians and several well-known celebrities weighed in; for example, actress Jenny McCarthy (who believed that a vaccination caused her son’s autism) co-authored a book on the matter. However, there is no scientific evidence that a link exists between autism and vaccinations (Hughes, 2007). Indeed, a recent study compared the vaccination histories of 256 children with autism spectrum disorder with that of 752 control children across three time periods during their first two years of life (birth to 3 months, birth to 7 months, and birth to 2 years) (DeStefano, Price, & Weintraub, 2013). At the time of the study, the children were between 6 and 13 years old, and their prior vaccination records were obtained. Because vaccines contain immunogens (substances that fight infections), the investigators examined medical records to see how many immunogens children received to determine if those children who received more immunogens were at greater risk for developing autism spectrum disorder. The results of this study, a portion of which are shown in Figure 15.19, clearly demonstrate that the quantity of immunogens from vaccines received during the first two years of life were not at all related to the development of autism spectrum disorder. There is not a relationship between vaccinations and autism spectrum disorders.
Why does concern over vaccines and autism spectrum disorder persist? Since the proliferation of the Internet in the 1990s, parents have been constantly bombarded with online information that can become magnified and take on a life of its own. The enormous volume of electronic information pertaining to autism spectrum disorder, combined with how difficult it can be to grasp complex scientific concepts, can make separating good research from bad challenging (Downs, 2008). Notably, the study that fueled the controversy reported that 8 out of 12 children—according to their parents—developed symptoms consistent with autism spectrum disorder shortly after receiving a vaccination. To conclude that vaccines cause autism spectrum disorder on this basis, as many did, is clearly incorrect for a number of reasons, not the least of which is because correlation does not imply causation, as you’ve learned.
Additionally, as was the case with diet and ADHD in the 1970s, the notion that autism spectrum disorder is caused by vaccinations is appealing to some because it provides a simple explanation for this condition. Like all disorders, however, there are no simple explanations for autism spectrum disorder. Although the research discussed above has shed some light on its causes, science is still a long way from a complete understanding of the disorder.
What are Learning Disabilities?
Learning disabilities are cognitive disorders that affect different areas of cognition, particularly language or reading. It should be pointed out that learning disabilities are not the same thing as intellectual disabilities. Learning disabilities are considered specific neurological impairments rather than global intellectual or developmental disabilities. A person with a language disability has difficulty understanding or using spoken language, whereas someone with a reading disability, such as dyslexia, has difficulty processing what he or she is reading.
Often, learning disabilities are not recognized until a child reaches school age. One confounding aspect of learning disabilities is that they most often affect children with average to above-average intelligence. In other words, the disability is specific to a particular area and not a measure of overall intellectual ability. At the same time, learning disabilities tend to exhibit comorbidity with other disorders, like attention-deficit hyperactivity disorder (ADHD). Anywhere between 30–70% of individuals with diagnosed cases of ADHD also have some sort of learning disability (Riccio, Gonzales, & Hynd, 1994). Let’s take a look at three examples of common learning disabilities: dysgraphia, dyslexia, and dyscalculia.
WHAT DO YOU THINK? Capital Punishment and Criminals with Intellectual Disabilities
The case of Atkins v. Virginia was a landmark case in the United States Supreme Court. On August 16, 1996, two men, Daryl Atkins and William Jones, robbed, kidnapped, and then shot and killed Eric Nesbitt, a local airman from the U.S. Air Force. A clinical psychologist evaluated Atkins and testified at the trial that Atkins had an IQ of 59. The mean IQ score is 100. The psychologist concluded that Atkins was mildly mentally retarded.
The jury found Atkins guilty, and he was sentenced to death. Atkins and his attorneys appealed to the Supreme Court. In June 2002, the Supreme Court reversed a previous decision and ruled that executions of mentally retarded criminals are ‘cruel and unusual punishments’ prohibited by the Eighth Amendment. The court wrote in their decision:
Clinical definitions of mental retardation require not only subaverage intellectual functioning, but also significant limitations in adaptive skills. Mentally retarded persons frequently know the difference between right and wrong and are competent to stand trial. Because of their impairments, however, by definition they have diminished capacities to understand and process information, to communicate, to abstract from mistakes and learn from experience, to engage in logical reasoning, to control impulses, and to understand others’ reactions. Their deficiencies do not warrant an exemption from criminal sanctions, but diminish their personal culpability (Atkins v. Virginia, 2002, par. 5).
The court also decided that there was a state legislature consensus against the execution of the mentally retarded and that this consensus should stand for all of the states. The Supreme Court ruling left it up to the states to determine their own definitions of mental retardation and intellectual disability. The definitions vary among states as to who can be executed. In the Atkins case, a jury decided that because he had many contacts with his lawyers and thus was provided with intellectual stimulation, his IQ had reportedly increased, and he was now smart enough to be executed. He was given an execution date and then received a stay of execution after it was revealed that lawyers for co-defendant, William Jones, coached Jones to “produce a testimony against Mr. Atkins that did match the evidence” (Liptak, 2008). After the revelation of this misconduct, Atkins was re-sentenced to life imprisonment.
Atkins v. Virginia (2002) highlights several issues regarding society’s beliefs around intelligence. In the Atkins case, the Supreme Court decided that intellectual disability does affect decision making and therefore should affect the nature of the punishment such criminals receive. Where, however, should the lines of intellectual disability be drawn? In May 2014, the Supreme Court ruled in a related case (Hall v. Florida) that IQ scores cannot be used as a final determination of a prisoner’s eligibility for the death penalty (Roberts, 2014).
Dysgraphia
Children with dysgraphia have a learning disability that results in a struggle to write legibly. The physical task of writing with a pen and paper is extremely challenging for the person. These children often have extreme difficulty putting their thoughts down on paper (Smits-Engelsman & Van Galen, 1997). This difficulty is inconsistent with a person’s IQ. That is, based on the child’s IQ and/or abilities in other areas, a child with dysgraphia should be able to write, but can’t. Children with dysgraphia may also have problems with spatial abilities.
Students with dysgraphia need academic accommodations to help them succeed in school. These accommodations can provide students with alternative assessment opportunities to demonstrate what they know (Barton, 2003). For example, a student with dysgraphia might be permitted to take an oral exam rather than a traditional paper-and-pencil test. Treatment is usually provided by an occupational therapist, although there is some question as to how effective such treatment is (Zwicker, 2005).
Dyslexia
Dyslexia is the most common learning disability in children. An individual with dyslexia exhibits an inability to correctly process letters. The neurological mechanism for sound processing does not work properly in someone with dyslexia. As a result, dyslexic children may not understand sound-letter correspondence. A child with dyslexia may mix up letters within words and sentences—letter reversals, such as those shown in Figure 7.17, are a hallmark of this learning disability—or skip whole words while reading. A dyslexic child may have difficulty spelling words correctly while writing. Because of the disordered way that the brain processes letters and sound, learning to read is a frustrating experience. Some dyslexic individuals cope by memorizing the shapes of most words, but they never actually learn to read (Berninger, 2008).
Dyscalculia
Dyscalculia is difficulty in learning or comprehending arithmetic. This learning disability is often first evident when children exhibit difficulty discerning how many objects are in a small group without counting them. Other symptoms may include struggling to memorize math facts, organize numbers, or fully differentiate between numerals, math symbols, and written numbers (such as “3” and “three”).
15.10 Personality Disorders
Learning Objectives
By the end of this section, you will be able to:
- Describe the nature of personality disorders and how they differ from other disorders
- List and distinguish between the three clusters of personality disorders
- Identify the basic features of borderline personality disorder and antisocial personality disorder, and the factors that are important in the etiology of both
The term personality refers loosely to one’s stable, consistent, and distinctive way of thinking about, feeling, acting, and relating to the world. People with personality disorders exhibit a personality style that differs markedly from the expectations of their culture, is pervasive and inflexible, begins in adolescence or early adulthood, and causes distress or impairment (APA, 2013). Generally, individuals with these disorders exhibit enduring personality styles that are extremely troubling and often create problems for them and those with whom they come into contact. Their maladaptive personality styles frequently bring them into conflict with others, disrupt their ability to develop and maintain social relationships, and prevent them from accomplishing realistic life goals.
The DSM-5 recognizes 10 personality disorders, organized into 3 different clusters. Cluster A disorders include paranoid personality disorder, schizoid personality disorder, and schizotypal personality disorder. People with these disorders display a personality style that is odd or eccentric. Cluster B disorders include antisocial personality disorder, histrionic personality disorder, narcissistic personality disorder, and borderline personality disorder. People with these disorders usually are impulsive, overly dramatic, highly emotional, and erratic. Cluster C disorders include avoidant personality disorder, dependent personality disorder, and obsessive-compulsive personality disorder (which is not the same thing as obsessive-compulsive disorder). People with these disorders often appear to be nervous and fearful. Table 15.2 provides a description of each of the DSM-5 personality disorders:
| DSM-5 Personality Disorders | ||
|---|---|---|
| DSM-5 Personality Disorder | Description | Cluster |
| Paranoid | harbors a pervasive and unjustifiable suspiciousness and mistrust of others; reluctant to confide in or become close to others; reads hidden demeaning or threatening meaning into benign remarks or events; takes offense easily and bears grudges; not due to schizophrenia or other psychotic disorders | A |
| Schizoid | lacks interest and desire to form relationships with others; aloof and shows emotional coldness and detachment; indifferent to approval or criticism of others; lacks close friends or confidants; not due to schizophrenia or other psychotic disorders, not an autism spectrum disorder | A |
| Schizotypal | exhibits eccentricities in thought, perception, emotion, speech, and behavior; shows suspiciousness or paranoia; has unusual perceptual experiences; speech is often idiosyncratic; displays inappropriate emotions; lacks friends or confidants; not due to schizophrenia or other psychotic disorder, or to autism spectrum disorder | A |
| Antisocial | continuously violates the rights of others; history of antisocial tendencies prior to age 15; often lies, fights, and has problems with the law; impulsive and fails to think ahead; can be deceitful and manipulative in order to gain profit or pleasure; irresponsible and often fails to hold down a job or pay financial debts; lacks feelings for others and remorse over misdeeds | B |
| Histrionic | excessively overdramatic, emotional, and theatrical; feels uncomfortable when not the center of others’ attention; behavior is often inappropriately seductive or provocative; speech is highly emotional but often vague and diffuse; emotions are shallow and often shift rapidly; may alienate friends with demands for constant attention | B |
| Narcissistic | overinflated and unjustified sense of self-importance and preoccupied with fantasies of success; believes he is entitled to special treatment from others; shows arrogant attitudes and behaviors; takes advantage of others; lacks empathy | B |
| Borderline | unstable in self-image, mood, and behavior; cannot tolerate being alone and experiences chronic feelings of emptiness; unstable and intense relationships with others; behavior is impulsive, unpredictable, and sometimes self-damaging; shows inappropriate and intense anger; makes suicidal gestures | B |
| Avoidant | socially inhibited and oversensitive to negative evaluation; avoids occupations that involve interpersonal contact because of fears of criticism or rejection; avoids relationships with others unless guaranteed to be accepted unconditionally; feels inadequate and views self as socially inept and unappealing; unwilling to take risks or engage in new activities if they may prove embarrassing | C |
| Dependent | allows others to take over and run her life; is submissive, clingy, and fears separation; cannot make decisions without advice and reassurance from others; lacks self-confidence; cannot do things on her own; feels uncomfortable or helpless when alone | C |
| Obsessive-Compulsive | pervasive need for perfectionism that interferes with the ability to complete tasks; preoccupied with details, rules, order, and schedules; excessively devoted to work at the expense of leisure and friendships; rigid, inflexible, and stubborn; insists things be done his way; miserly with money | C |
Slightly over 9% of the U.S. population suffers from a personality disorder, with avoidant and schizoid personality disorders the most frequent (Lezenweger, Lane, Loranger, & Kessler, 2007). Two of these personality disorders, borderline personality disorder and antisocial personality disorder, are regarded by many as especially problematic.
Borderline Personality Disorder
The “borderline” in borderline personality disorder was originally coined in the late 1930s in an effort to describe patients who appeared anxious, but were prone to brief psychotic experiences—that is, patients who were thought to be literally on the borderline between anxiety and psychosis (Freeman, Stone, Martin, & Reinecke, 2005). Today, borderline personality disorder has a completely different meaning. Borderline personality disorder is characterized chiefly by instability in interpersonal relationships, self-image, and mood, as well as marked impulsivity (APA, 2013). People with borderline personality disorder cannot tolerate the thought of being alone and will make frantic efforts (including making suicidal gestures and engaging in self-mutilation) to avoid abandonment or separation (whether real or imagined). Their relationships are intense and unstable; for example, a lover may be idealized early in a relationship, but then later vilified at the slightest sign she appears to no longer show interest. These individuals have an unstable view of self and, thus, might suddenly display a shift in personal attitudes, interests, career plans, and choice of friends. For example, a law school student may, despite having invested tens of thousands of dollars toward earning a law degree and despite having performed well in the program, consider dropping out and pursuing a career in another field. People with borderline personality disorder may be highly impulsive and may engage in reckless and self-destructive behaviors such as excessive gambling, spending money irresponsibly, substance abuse, engaging in unsafe sex, and reckless driving. They sometimes show intense and inappropriate anger that they have difficulty controlling, and they can be moody, sarcastic, bitter, and verbally abusive.
The prevalence of borderline personality disorder in the U.S. population is estimated to be around 1.4% (Lezenweger et al., 2007), but the rates are higher among those who use mental health services; approximately 10% of mental health outpatients and 20% of psychiatric inpatients meet the criteria for diagnosis (APA, 2013). Additionally, borderline personality disorder is comorbid with anxiety, mood, and substance use disorders (Lezenweger et al., 2007).
Biological Basis for Borderline Personality Disorder
Genetic factors appear to be important in the development of borderline personality disorder. For example, core personality traits that characterize this disorder, such as impulsivity and emotional instability, show a high degree of heritability (Livesley, 2008). Also, the rates of borderline personality disorder among relatives of people with this disorder have been found to be as high as 24.9% (White, Gunderson, Zanarani, & Hudson, 2003). Individuals with borderline personality disorder report experiencing childhood physical, sexual, and/or emotional abuse at rates far greater than those observed in the general population (Afifi et al., 2010), indicating that environmental factors are also crucial. These findings would suggest that borderline personality disorder may be determined by an interaction between genetic factors and adverse environmental experiences. Consistent with this hypothesis, one study found that the highest rates of borderline personality disorder were among individuals with a borderline temperament (characterized by high novelty seeking and high harm-avoidance) and those who experienced childhood abuse and/or neglect (Joyce et al., 2003).
Antisocial Personality Disorder
Most human beings live in accordance with a moral compass, a sense of right and wrong. Most individuals learn at a very young age that there are certain things that should not be done. We learn that we should not lie or cheat. We are taught that it is wrong to take things that do not belong to us, and that it is wrong to exploit others for personal gain. We also learn the importance of living up to our responsibilities, of doing what we say we will do. People with antisocial personality disorder, however, do not seem to have a moral compass. These individuals act as though they neither have a sense of nor care about right or wrong. Not surprisingly, these people represent a serious problem for others and for society in general.
According to the DSM-5, the individual with antisocial personality disorder shows no regard at all for other people’s rights or feelings. This lack of regard is exhibited a number of ways and can include repeatedly performing illegal acts, lying to or conning others, impulsivity and recklessness, irritability and aggressiveness toward others, and failure to act in a responsible way (e.g., leaving debts unpaid) (APA, 2013). The worst part about antisocial personality disorder, however, is that people with this disorder have no remorse over their misdeeds; these people will hurt, manipulate, exploit, and abuse others and not feel any guilt. Signs of this disorder can emerge early in life; however, a person must be at least 18 years old to be diagnosed with antisocial personality disorder.
People with antisocial personality disorder seem to view the world as self-serving and unkind. They seem to think that they should use whatever means necessary to get by in life. They tend to view others not as living, thinking, feeling beings, but rather as pawns to be used or abused for a specific purpose. They often have an over-inflated sense of themselves and can appear extremely arrogant. They frequently display superficial charm; for example, without really meaning it they might say exactly what they think another person wants to hear. They lack empathy: they are incapable of understanding the emotional point-of-view of others. People with this disorder may become involved in illegal enterprises, show cruelty toward others, leave their jobs with no plans to obtain another job, have multiple sexual partners, repeatedly get into fights with others, and show reckless disregard for themselves and others (e.g., repeated arrests for driving while intoxicated) (APA, 2013).
The DSM-5 has included an alternative model for conceptualizing personality disorders based on the traits identified in the Five Factor Model of personality. This model addresses the level of personality functioning such as impairments in self (identity or self-direction) and interpersonal (empathy or intimacy) functioning. In the case of antisocial personality disorder, the DSM-5 identifies the predominant traits of antagonism (such as disregard for others’ needs, manipulative or deceitful behavior) and disinhibition (characterized by impulsivity, irresponsibility, and risk-taking) (Harwood, Schade, Krueger, Wright, & Markon, 2012). A psychopathology specifier is also included that emphasizes traits such as attention seeking and low anxiousness (lack of concern about negative consequences for risky or harmful behavior) (Crego & Widiger, 2014).
Risk Factors for Antisocial Personality Disorder
Antisocial personality disorder is observed in about 3.6% of the population; the disorder is much more common among males, with a 3 to 1 ratio of men to women, and it is more likely to occur in men who are younger, widowed, separated, divorced, of lower socioeconomic status, who live in urban areas, and who live in the western United States (Compton, Conway, Stinson, Colliver, & Grant, 2005). Compared to men with antisocial personality disorder, women with the disorder are more likely to have experienced emotional neglect and sexual abuse during childhood, and they are more likely to have had parents who abused substances and who engaged in antisocial behaviors themselves (Alegria et al., 2013).
Table 15.3 shows some of the differences in the specific types of antisocial behaviors that men and women with antisocial personality disorder exhibit (Alegria et al., 2013).
| Gender Differences in Antisocial Personality Disorder | |
|---|---|
| Men with antisocial personality disorder are more likely than women with antisocial personality disorder to | Women with antisocial personality disorder are more likely than men with antisocial personality to |
|
|
Family, twin, and adoption studies suggest that both genetic and environmental factors influence the development of antisocial personality disorder, as well as general antisocial behavior (criminality, violence, aggressiveness) (Baker, Bezdjian, & Raine, 2006). Personality and temperament dimensions that are related to this disorder, including fearlessness, impulsive antisociality, and callousness, have a substantial genetic influence (Livesley & Jang, 2008). Adoption studies clearly demonstrate that the development of antisocial behavior is determined by the interaction of genetic factors and adverse environmental circumstances (Rhee & Waldman, 2002). For example, one investigation found that adoptees of biological parents with antisocial personality disorder were more likely to exhibit adolescent and adult antisocial behaviors if they were raised in adverse adoptive family environments (e.g., adoptive parents had marital problems, were divorced, used drugs, and had legal problems) than if they were raised in a more normal adoptive environment (Cadoret, Yates, Ed, Woodworth, & Stewart, 1995).
Researchers who are interested in the importance of environment in the development of antisocial personality disorder have directed their attention to such factors as the community, the structure and functioning of the family, and peer groups. Each of these factors influences the likelihood of antisocial behavior. One longitudinal investigation of more than 800 Seattle-area youth measured risk factors for violence at 10, 14, 16, and 18 years of age (Herrenkohl et al., 2000). The risk factors examined included those involving the family, peers, and community. A portion of the findings from this study are provided in Figure 15.20.
Those with antisocial tendencies do not seem to experience emotions the way most other people do. These individuals fail to show fear in response to environment cues that signal punishment, pain, or noxious stimulation. For instance, they show less skin conductance (sweatiness on hands) in anticipation of electric shock than do people without antisocial tendencies (Hare, 1965). Skin conductance is controlled by the sympathetic nervous system and is used to assess autonomic nervous system functioning. When the sympathetic nervous system is active, people become aroused and anxious, and sweat gland activity increases. Thus, increased sweat gland activity, as assessed through skin conductance, is taken as a sign of arousal or anxiety. For those with antisocial personality disorder, a lack of skin conductance may indicate the presence of characteristics such as emotional deficits and impulsivity that underlie the propensity for antisocial behavior and negative social relationships (Fung et al., 2005).
Another example showing that those with antisocial personality disorder fail to respond to environmental cues comes from a recent study by Stuppy-Sullivan and Baskin-Sommers (2019). The researchers studied cognitive and reward factors associated with antisocial personality disorder dysfunction in 119 incarcerated males. Each subject was administered three tasks targeting different aspects of cognition and reward. High-magnitude rewards tended to impair perception in those with antisocial personality disorder, worsened executive function when they were consciously aware of the high rewards, and worsened inhibition when the tasks placed high demand on working memory.
Chapter Highlights
Psychological disorders are syndromes characterized by clinically significant disturbances in an individual’s cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underlying mental functioning. There are specific strategies used to provide diagnoses, oftentimes utilizing a classification system such as the DSM-5 or ICD-10. The ways in which the world views psychological disorders today has not always been the most common perspective–a supernatural origin of explanation has developed into a mix of biology, genetics, and environmental factors. Some of the larger classifications that disordered behaviors fall into are anxiety disorders, obsessive-compulsive and related disorders, posttraumatic stress disorder, mood and related disorders, schizophrenia, dissociative disorders, developmental disorders, and personality disorders.
- Conceptualizing psychological disorders is difficult. It can be helpful to think of these disorders as atypical, distressful, and dysfunctional; however, not all behaviors that fall under any of these categories are considered to be psychopathology.
- Psychological disorders have varied interpretations according to different cultures.
- To maintain a consistent basis for diagnosis, classification systems such as the DSM and ICD are used. These diagnostic tools change are adapted as more becomes known about psychological disorders.
- Psychological disorders were once highly stigmatized with connections to devils, witches, and other demonic and supernatural forces.
- Current explanations for psychological disorders include biological factors and the diathesis-stress model–a combination of genetic and psychosocial attributes that foster the development of psychopathological concerns.
- Anxiety disorders induce disturbances in behavior due to an excessive and persistent feeling of fear and anxiety. Specific phobias, social anxiety disorder, panic disorder, and generalized anxiety disorder are all examples of anxiety disorders that are typically acquired and maintained through principles of learning and conditioning.
- Obsessive-compulsive and related disorders are characterized by intrusive, unpleasant thoughts (obsessions) and repetitive behaviors (compulsions). Disorders related to obsessive-compulsive disorder (OCD) are body dysmorphic disorder and hoarding disorder, established by classical conditioning and prolonged by operant conditioning.
- Flashbacks, persistent negative emotion, jumpiness, irritability, and other symptoms present for at least one month after a traumatic event describe posttraumatic stress disorder (PTSD).
- Risk factors for PTSD include violence, assault, neglect, death, injury, near-death experiences, combat, and natural disasters.
- Mood disorders are based on the presence of depressive and manic episodes and symptoms that create a difficulty in functioning. Depressive disorders and bipolar disorders are the primary diagnoses with subtypes such as, seasonal pattern, peripartum onset, or rapid-cycling, for example.
- A specific type of psychosis, schizophrenia, is characterized by a disturbance in thought, perception, emotion, and behavior, prevalent in nearly 1% of the population. Genetic linkages with schizophrenia are strong, but enlarged ventricles, neurotransmitter levels, marijuana use, and pregnancy complications can also influence the presence of the disorder.
- Prodromal symptoms of schizophrenia are predictors of a future development of the disorder; identification of these symptoms and proper treatment can aid in methods of mitigation.
- Dissociative amnesia, dissociative fugue, depersonalization/derealization disorder, and dissociative identity disorder are all dissociative disorders in which individuals become disconnected from their own sense of self. A desire to escape traumatic and emotional experiences is suggested as a reason for experiencing dissociation in these cases.
- Attention deficit/hyperactivity disorder is described by an increase in activity, difficulty concentrating, and increased impulsivity, occurring in 8% of children and limiting social and academic functioning.
- Autism spectrum disorder is based on hindered social functioning and communication in addition to repetitive behaviors and interests.
- Dysgraphia, dyscalculia, and dyslexia describe a difficulty writing, difficulty interpreting arithmetic, and difficulty comprehending letters and reading, respectively. These learning disabilities make school extremely challenging for children because they are neurological impairments that are difficult to treat.
- Split into three primary categories, personality disorders encompass a wide variety of persistent and destructive personality traits that begin in adolescence or early adulthood and hinder the development of healthy social relationships and accomplishing life goals.
- Currently there are ten personality disorders, grouped into three clusters: odd and eccentric (cluster A), dramatic, emotional, and erratic (cluster B), and anxious and fearful (cluster C).
End of Chapter Quiz
a condition characterized by abnormal thoughts, feelings, and behaviors
cause or causes of a psychological disorder
study of psychological disorders, including their symptoms, causes, and treatment; manifestation of a psychological disorder
describes behaviors or feelings that deviate from the norm
model of psychological disorders resulting from the inability of an internal mechanism to perform its natural function
determination of which disorder a set of symptoms represents
authoritative index of mental disorders and the criteria for their diagnosis; published by the American Psychiatric Association (APA)
co-occurrence of two disorders in the same individual
authoritative index of mental and physical diseases, including infectious diseases, and the criteria for their diagnosis; published by the World Health Organization (WHO)
describes a force beyond scientific understanding
suggests that people with a predisposition for a disorder (a diathesis) are more likely to develop the disorder when faced with stress; model of psychopathology
characterized by excessive and persistent fear and anxiety, and by related disturbances in behavior
anxiety disorder characterized by excessive, distressing, and persistent fear or anxiety about a specific object or situation
anxiety disorder characterized by intense fear, anxiety, and avoidance of situations in which it might be difficult to escape if one experiences symptoms of a panic attack
characterized by extreme and persistent fear or anxiety and avoidance of social situations in which one could potentially be evaluated negatively by others
mental and behavior acts designed to reduce anxiety in social situations by reducing the chance of negative social outcomes; common in social anxiety disorder
anxiety disorder characterized by unexpected panic attacks, along with at least one month of worry about panic attacks or self-defeating behavior related to the attacks
period of extreme fear or discomfort that develops abruptly; symptoms of panic attacks are both physiological and psychological
area of the brainstem that contains norepinephrine, a neurotransmitter that triggers the body’s fight-or-flight response; has been implicated in panic disorder
characterized by a continuous state of excessive, uncontrollable, and pointless worry and apprehension
group of overlapping disorders listed in the DSM-5 that involves intrusive, unpleasant thoughts and/or repetitive behaviors
characterized by the tendency to experience intrusive and unwanted thoughts and urges (obsession) and/or the need to engage in repetitive behaviors or mental acts (compulsions) in response to the unwanted thoughts and urges
involves excessive preoccupation with an imagined defect in physical appearance
characterized by persistent difficulty in parting with possessions, regardless of their actual value or usefulness
area of the frontal lobe involved in learning and decision-making
experiencing a profoundly traumatic event leads to a constellation of symptoms that include intrusive and distressing memories of the event, avoidance of stimuli connected to the event, negative emotional states, feelings of detachment from others, irritability, proneness toward outbursts, hypervigilance, and a tendency to startle easily; these symptoms must occur for at least one month.
one of a group of mood disorders in which depression is the defining feature
group of mood disorders in which mania is the defining feature
state of extreme elation and agitation
commonly referred to as “depression” or “major depression,” characterized by sadness or loss of pleasure in usual activities, as well other symptoms
thoughts of death by suicide, thinking about or planning suicide, or making a suicide attempt
subtype of depression in which a person experiences the symptoms of major depressive disorder only during a particular time of year
subtype of depression that applies to women who experience an episode of major depression either during pregnancy or in the four weeks following childbirth
depressive disorder characterized by a chronically sad and melancholy mood
mood disorder characterized by mood states that vacillate between depression and mania
period in which an individual experiences mania, characterized by extremely cheerful and euphoric mood, excessive talkativeness, irritability, increased activity levels, and other symptoms
symptom of mania that involves an abruptly switching in conversation from one topic to another
cognitive theory of depression proposing that a style of thinking that perceives negative life events as having stable and global causes leads to a sense of hopelessness and then to depression
death caused by intentional, self-directed injurious behavior
severe disorder characterized by major disturbances in thought, perception, emotion, and behavior with symptoms that include hallucinations, delusions, disorganized thinking and behavior, and negative symptoms
perceptual experience that occurs in the absence of external stimulation, such as the auditory hallucinations (hearing voices) common to schizophrenia
belief that is contrary to reality and is firmly held, despite contradictory evidence
characterized by beliefs that others are out to harm them
characterized by beliefs that one holds special power, unique knowledge, or is extremely important
belief that something highly unusual is happening to one’s body or internal organs
disjointed and incoherent thought processes, usually detected by what a person says
decreased reactivity to the environment; includes posturing and catatonic stupor
characterized by decreases and absences in certain normal behaviors, emotions, or drives, such as an expressionless face, lack of motivation to engage in activities, reduced speech, lack of social engagement, and inability to experience pleasure
theory of schizophrenia that proposes that an overabundance of dopamine or dopamine receptors is responsible for the onset and maintenance of schizophrenia
one of the fluid-filled cavities within the brain
in schizophrenia, one of the early minor symptoms of psychosis
group of DSM-5 disorders in which the primary feature is that a person becomes dissociated, or split off, from their core sense of self, resulting in disturbances in identity and memory
dissociative disorder characterized by an inability to recall important personal information, usually following an extremely stressful or traumatic experience
symptom of dissociative amnesia in which a person suddenly wanders away from one’s home and experiences confusion about their identity
dissociative disorder in which people feel detached from the self (depersonalization), and the world feels artificial and unreal (derealization)
dissociative disorder (formerly known as multiple personality disorder) in which a person exhibits two or more distinct, well-defined personalities or identities and experiences memory gaps for the time during which another identity emerged
one of the disorders that are first diagnosed in childhood and involve developmental problems in academic, intellectual, social functioning
childhood disorder characterized by inattentiveness and/or hyperactive, impulsive behavior
childhood disorder characterized by deficits in social interaction and communication, and repetitive patterns of behavior or interests
learning disability that causes extreme difficulty in writing legibly
common learning disability in which letters are not processed properly by the brain
learning disability that causes difficulty in learning or comprehending mathematics
group of DSM-5 disorders characterized by an inflexible and pervasive personality style that differs markedly from the expectations of one’s culture and causes distress and impairment; people with these disorders have a personality style that frequently brings them into conflict with others and disrupts their ability to develop and maintain social relationships
instability in interpersonal relationships, self-image, and mood, as well as impulsivity; key features include intolerance of being alone and fear of abandonment, unstable relationships, unpredictable behavior and moods, and intense and inappropriate anger
characterized by a lack of regard for others’ rights, impulsivity, deceitfulness, irresponsibility, and lack of remorse over misdeeds


